CLASSIFICATION OF PERIODONTAL DISEASE/GUM DISEASE
Periodontal Disease/Gum Disease
- What is the difference between Gingivitis and Periodontitis?
- What are the causes of Gum disease?
- Spot the 7 signs of Gum disease?
- How does Periodontist vs Dentist diagnose Gum disease?
- How is periodontal disease or Gum disease treated?
- How can Gum disease be prevented?
- Is Gum disease linked to other Systemic health problems?
Periodontics is an area of expertise that deals with treatment of the gum and bone supporting the teeth.
In health, the gums firmly grip the neck of the tooth. If food is allowed to accumulate between the tooth and the gum margin, it forms plaque along with the microbes. The resultant irritation of the gum margins produces a condition called as GINGIVITIS characterized by redness, bleeding and swelling of the gums. If proper attention is paid at this stage the condition is perfectly reversible. However in untreated cases the condition further deteriorates leading to the destruction of the tooth-supporting tissues. The condition is then called PERIODONTITIS or PYORRHOEA. At this stage the teeth start shaking, they are unable to withstand chewing forces, pus forms in the gums and foul smell starts from the mouth.
Periodontitis also called Gum disease or Periodontal disease begins with bacterial growth (Plaque) in our oral cavity and may cause tooth loss (if not properly treated) due to destruction of the tissues (Periodontium) that surrounds our teeth.
What’s the Difference Between Gingivitis and Periodontitis?
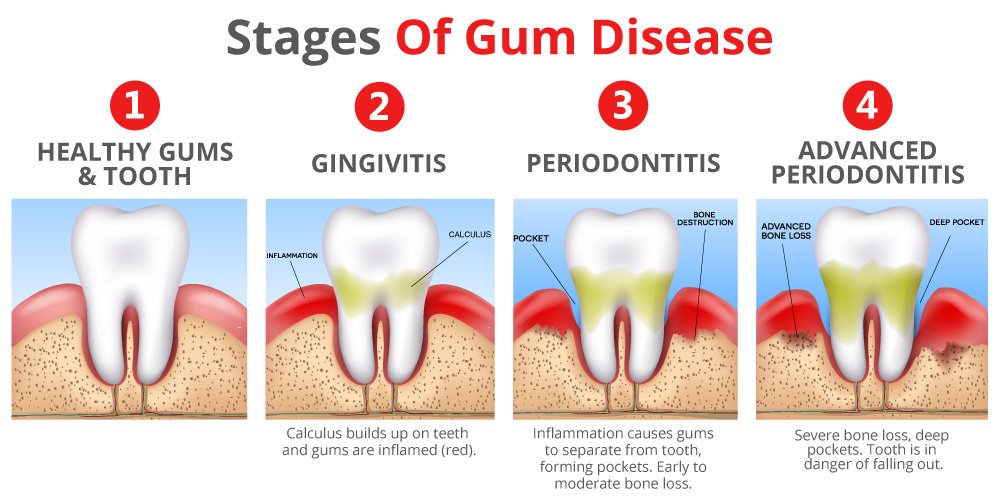
Gingivitis (Gum inflammation) is the initial stage of gum disease and usually precedes periodontitis. However, it is important to note that not all gingivitis cases progress to periodontitis.
In the early stage of gingivitis, bacteria in plaque build up, causing the gums to become inflamed (red, swollen & bleed easily during tooth brushing). No irreversible bone or other tissue damage has occurred at this stage.
When gingivitis is left untreated, it can advance to periodontitis. In a person with periodontitis, the inner layer of the gum gets pulled away from the teeth and form periodontal pockets (Pseudo or true Pocket) with or without loss of supporting bone. These pockets or small spaces between teeth and gums collect debris and can become infected. The body’s immune system fights against the bacteria as the plaque spreads and grows below the gum line.
Toxins or poisons produced by the bacteria in plaque, tarter & calculus as well as the body’s own immune mechanism (Host immune response) involved in fighting infections start to break down the bone and connective tissue that hold teeth in place. As the disease progresses, the pockets deepen and more gum tissue and bone are destroyed. When this happens, teeth are no longer anchored in place, they become loose or mobile, and tooth loss occurs. Gum disease is the leading cause of tooth loss in adults.
What Causes Gum Disease?
Plaque is the primary cause of gum disease. However, other factors can contribute to periodontal disease. These include:
- Hormonal changes, such as those occurring during pregnancy, puberty, menopause, and monthly menstruation, make gums more sensitive, which makes it easier for gingivitis to develop.
- Illnesses may affect the condition of your gums. This includes diseases such as cancer or HIV that interfere with the immune system. Because diabetes affects the body’s ability to use blood sugar, patients with this disease are at higher risk of developing infections, including periodontal disease and cavities.
- Medications can affect oral health, because some lessen the flow of saliva, which has a protective effect on teeth and gums. Some drugs, such as the anticonvulsant medication Dilantin and the anti-angina drug Procardia and Adalat, can cause abnormal growth of gum tissue.
- Bad habits such as smoking make it harder for gum tissue to repair itself.
- Poor oral hygiene habits such as not brushing and flossing on a daily basis, make it easier for gingivitis to develop.
- Family history of dental disease can be a contributing factor for the development of gingivitis.
What Are the Symptoms of Gum Disease?
Gum disease may progress painlessly, producing few obvious signs, even in the late stages of the disease. Although the symptoms of periodontal disease often are subtle, the condition is not entirely without warning signs. Certain symptoms may point to some form of the disease. The symptoms of gum disease include:
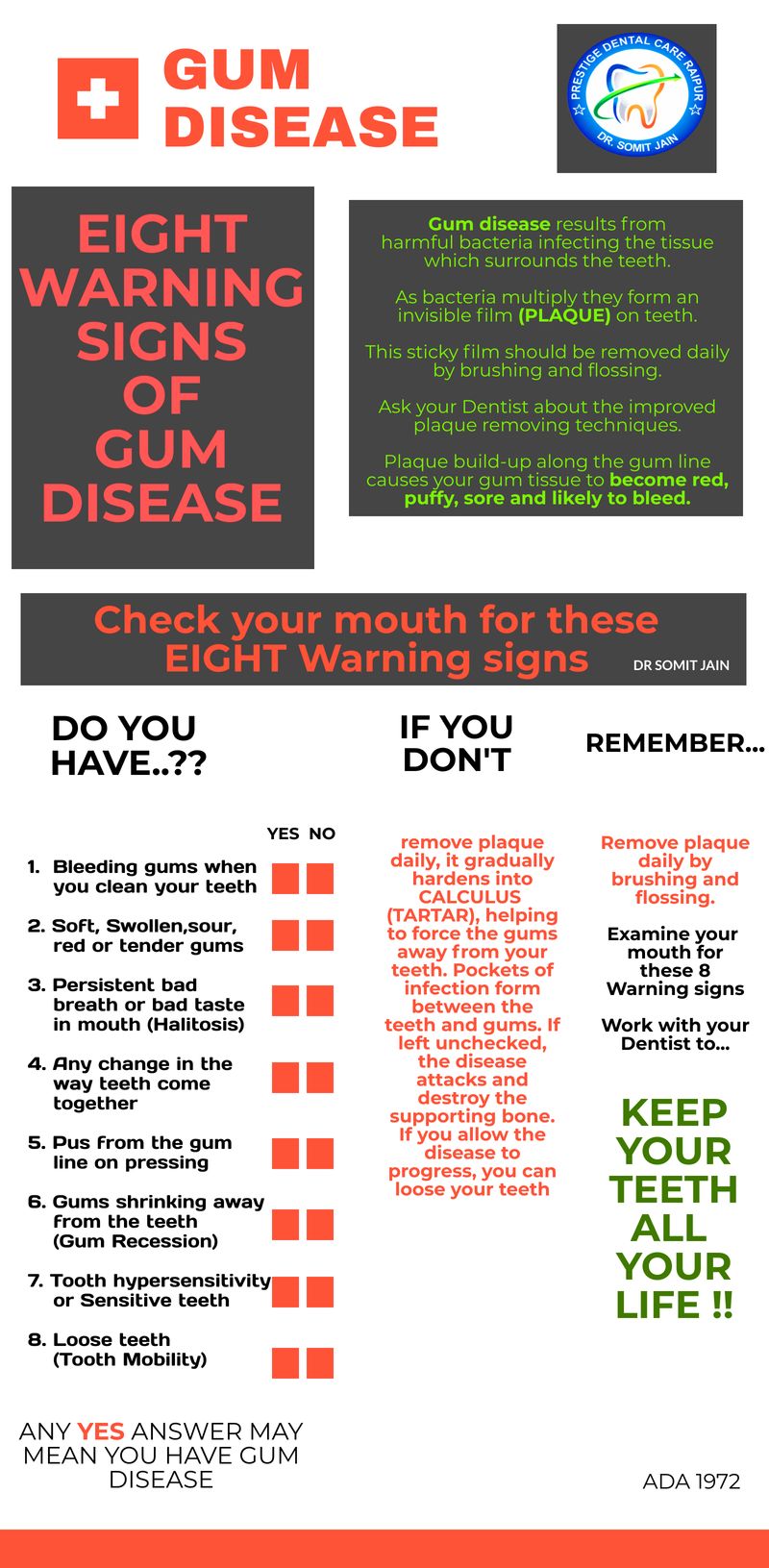
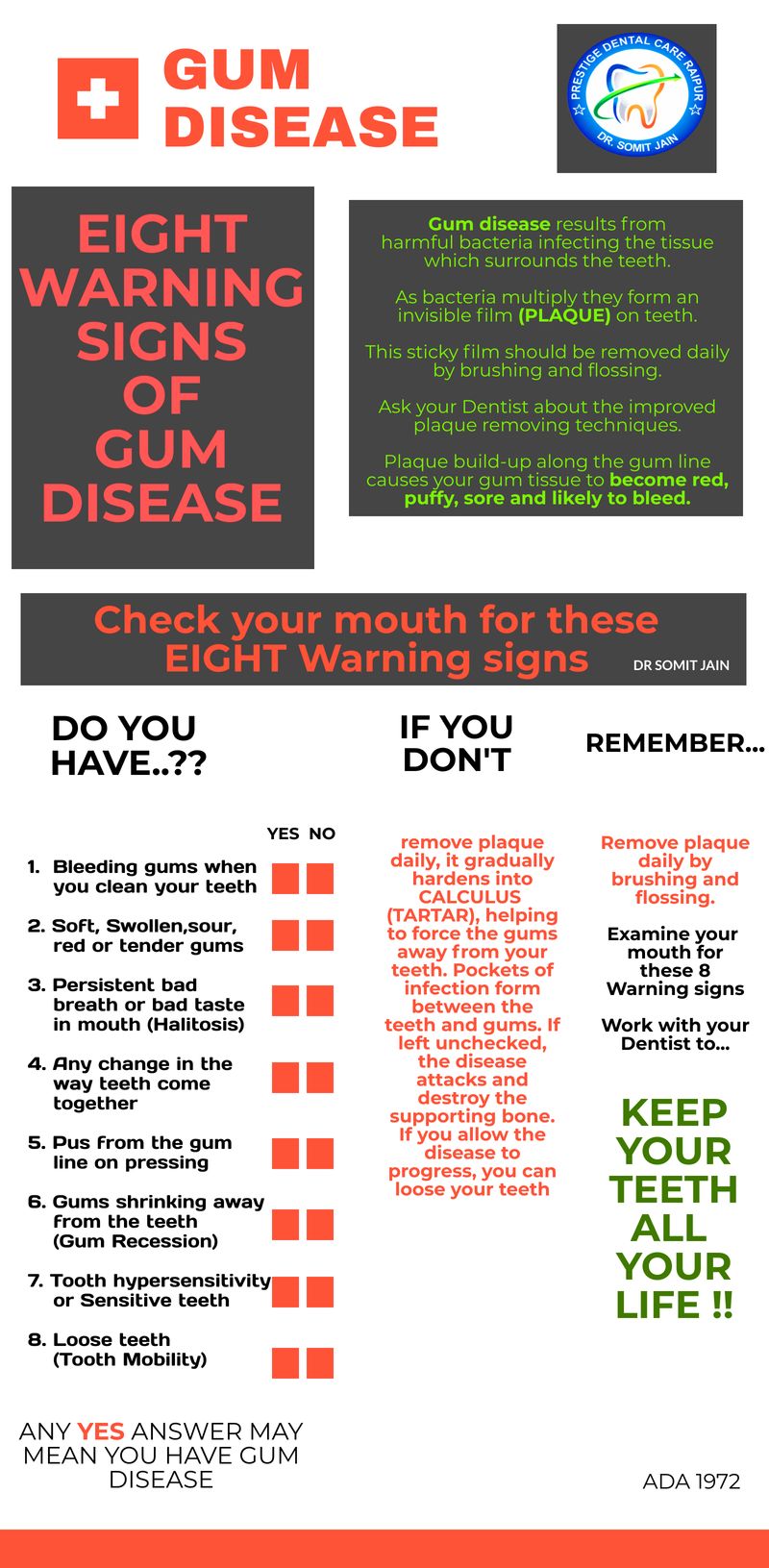
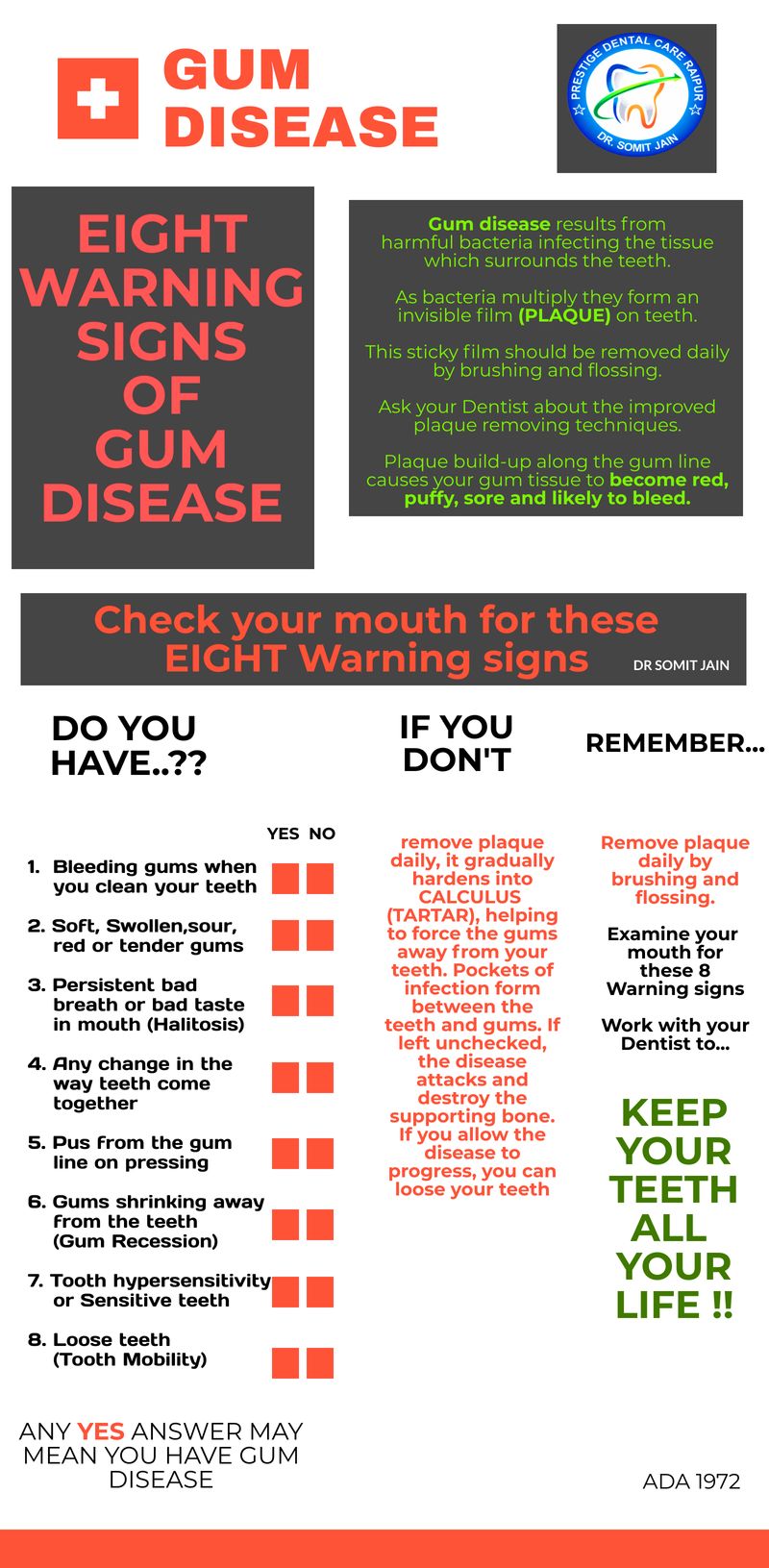
Spot the 8 signs of gum disease (Dr Somit Jain, Gum specialist Periodontist near me)
- Gums that bleed during and after tooth brushing
- Red, swollen, or tender gums
- Persistent bad breath or bad taste in the mouth
- Receding gums
- Formation of deep pockets between teeth and gums
- Loose or shifting teeth
- Changes in the way teeth fit together upon biting down, or in the fit of partial dentures.
Even if you don’t notice any symptoms, you may still have some degree of gum disease. In some people, gum disease may affect only certain teeth, such as the molars. Only a dentist or a periodontist can recognize and determine the progression of gum disease.
How Does My Periodontist Diagnose Gum Disease?
During a Periodontal examination, your Periodontist typically checks for these things:
- Bleeding gums (Bleeding on probing), swelling, firmness, pocket depth (the space between the gum and tooth; the larger and deeper the pocket, the more severe the disease), loss of attachment, furcation involvement.
- Teeth mobility and tooth sensitivity, proper teeth alignment (pathological migration) and trauma from occlusion (TFO)
- Radiographic examination including Dental X-Ray
- Intraoral Periapical Radiography (IOPA)
- OPG (Orthopantomogram)
How Is Gum Disease Treated?
- Goals to promote reattachment of healthy gums to teeth; reduce redness, swelling, bleeding gums, depth of pockets and to stop disease progression.
- Treatment options depend on the stage of disease, response to earlier gum treatments, and your overall health.
- Options range from Nonsurgical Periodontal therapies that control bacterial growth to Surgical Periodontal therapies to restore supportive tissues. A full description of the various treatment options has been presented in Gum Disease Treatments.
How Can Gum Disease Be Prevented?
- Gingivitis can be reversed and the progression of gum disease can be stopped in nearly all cases when proper plaque control is practiced.
- Proper plaque control consists of Professional cleanings at least once a year and daily brushing (twice daily) and flossing.
- Brushing eliminates plaque from the surfaces of the teeth that can be reached; flossing removes food particles and plaque from in between the teeth and under the gum line.
- Antibacterial mouth rinses can reduce bacteria that cause plaque and gum disease, according to the Indian Society of Periodontology.
- Warm saline rinses (2-4 times/day)
Other health and lifestyle changes that will decrease the risk, severity, and speed of gum disease development include:
- Stop smoking. Tobacco use is a significant risk factor for development of periodontitis. Smokers are seven times more likely to get gum disease than nonsmokers, and smokingcan lower the chances of success of some treatments.
- Reduce stress . Stress may make it difficult for your body’s immune system to fight off infection.
- Maintain a well-balanced diet. Proper nutrition helps your immune system fight infection. Eating foods with antioxidant properties — for example, those containing vitamin E ( vegetable oils, nuts, green leafy vegetables) and vitamin C (citrus fruits, broccoli, potatoes) — can help your body repair damaged tissue.
- Avoid clenching and grinding your teeth. These actions may put excess force on the supporting tissues of the teeth and could increase the rate at which these tissues are destroyed.
Despite following good oral hygiene practices and making other healthy lifestyle choices, the American Academy of Periodontology says that up to 30% of Americans may be genetically susceptible to gum disease. And those who are genetically predisposed may be up to six times more likely to develop some form of gum disease. If anyone in your family has gum disease, it may mean that you are at greater risk, as well. If you are more susceptible to gum disease, your dentist or periodontist may recommend more frequent check-ups, cleanings, and treatments to better manage the condition.
What are the Warning signs of Gum Disease??



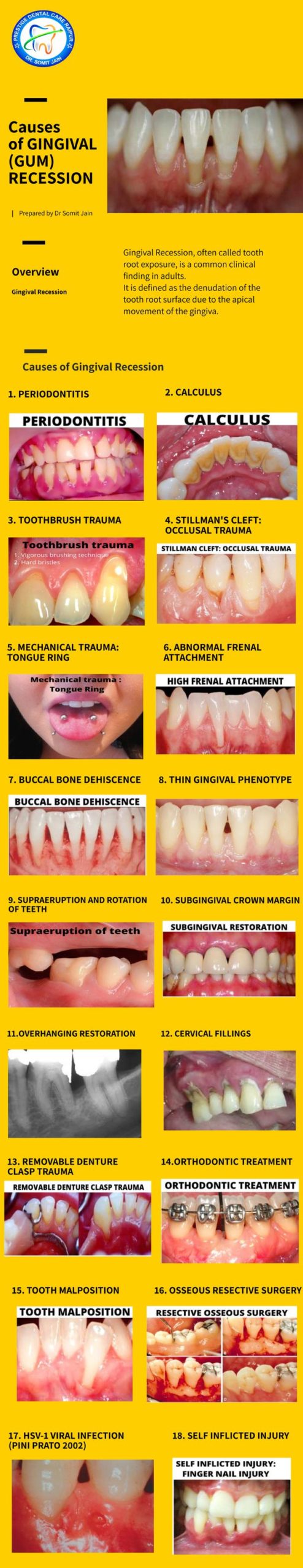
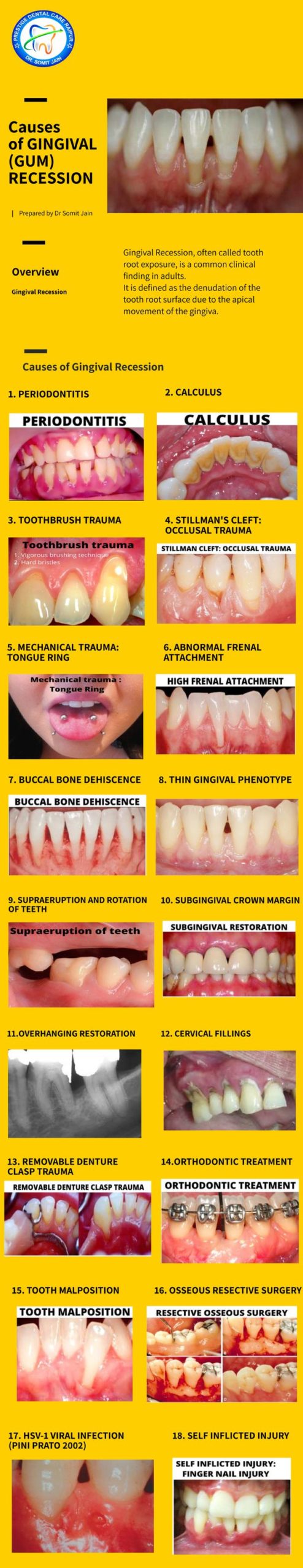
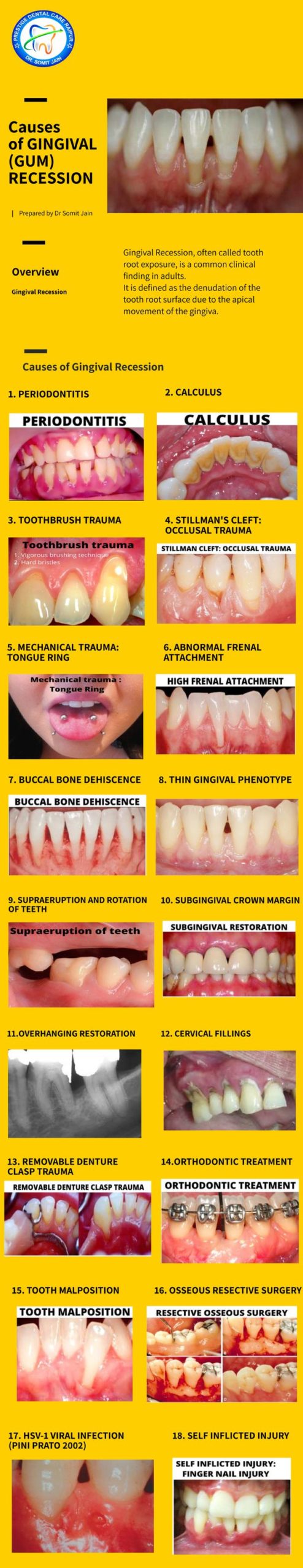
What are the causes of Gingival (Gum) Recession..??