1#. Key Points
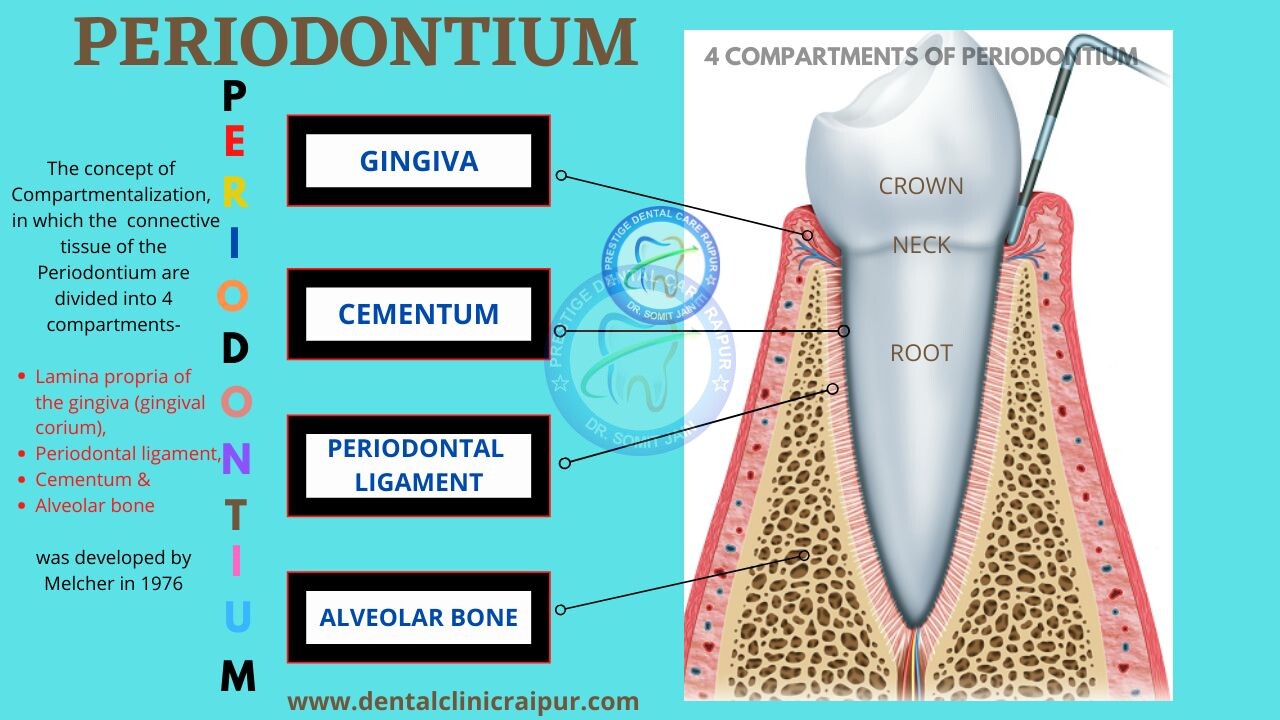
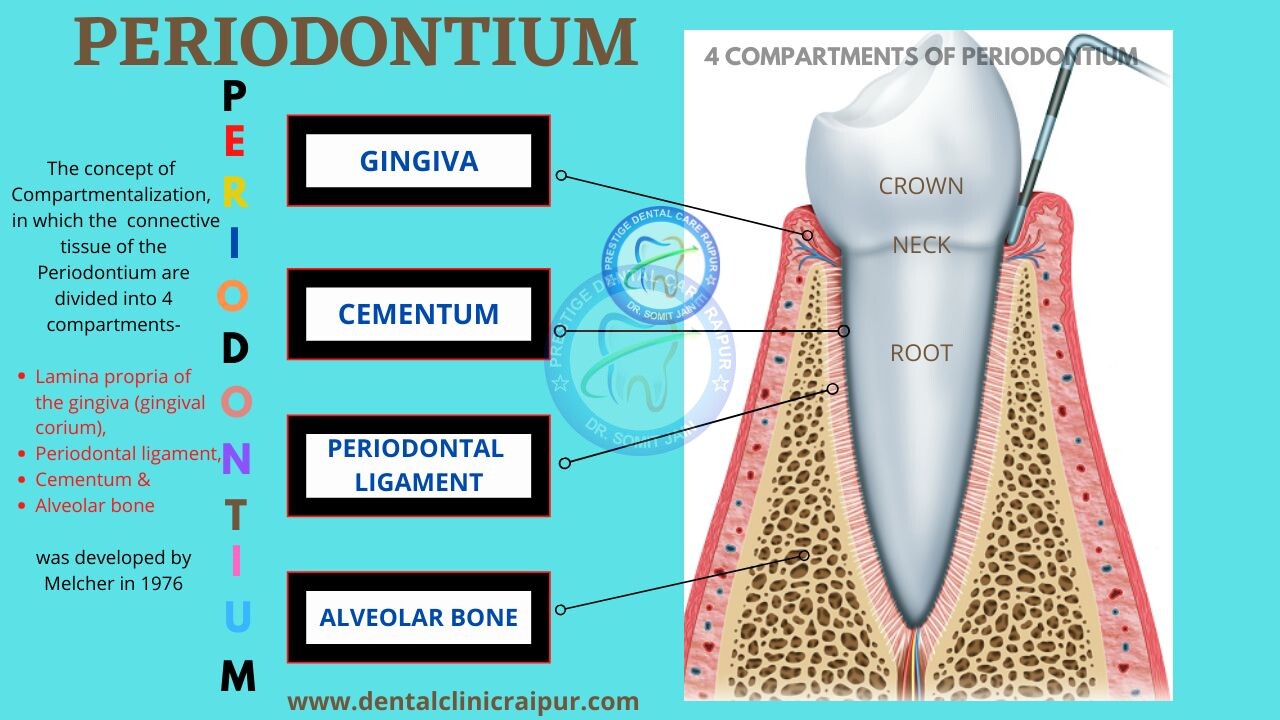
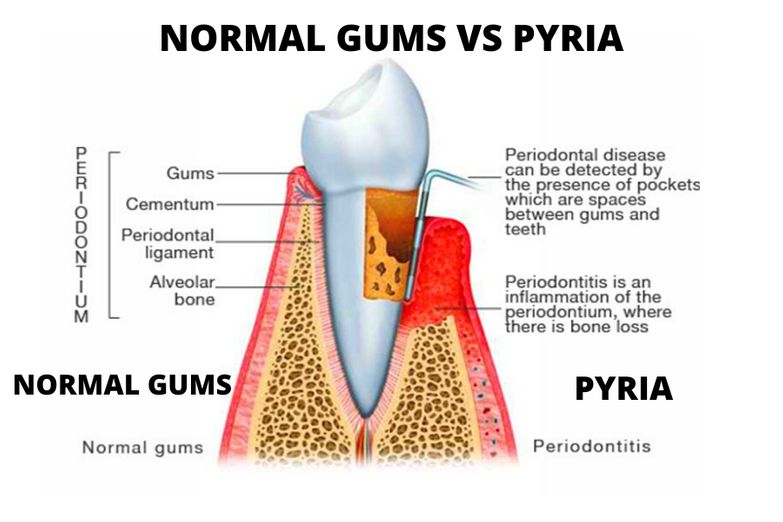
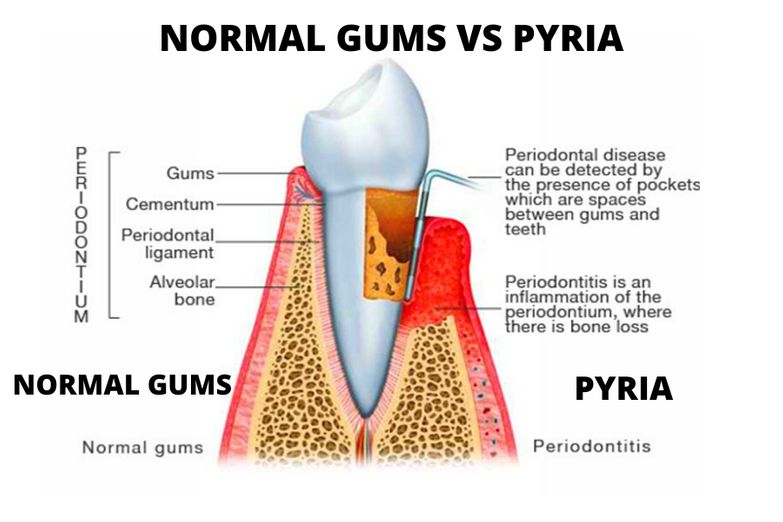
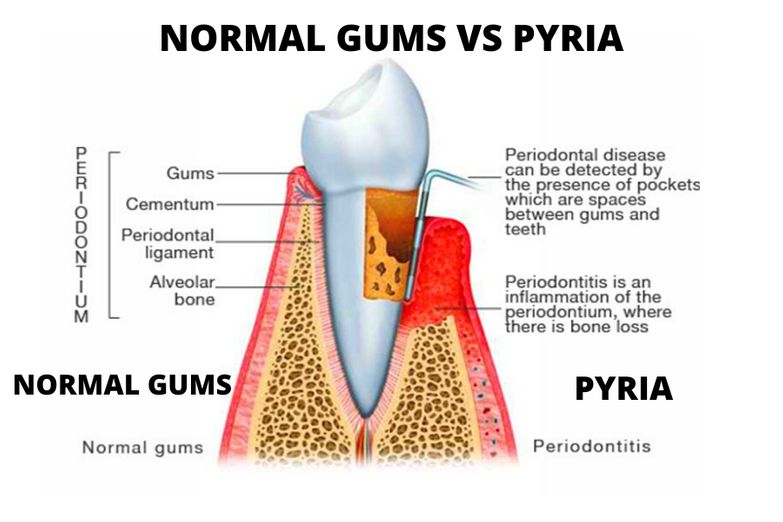
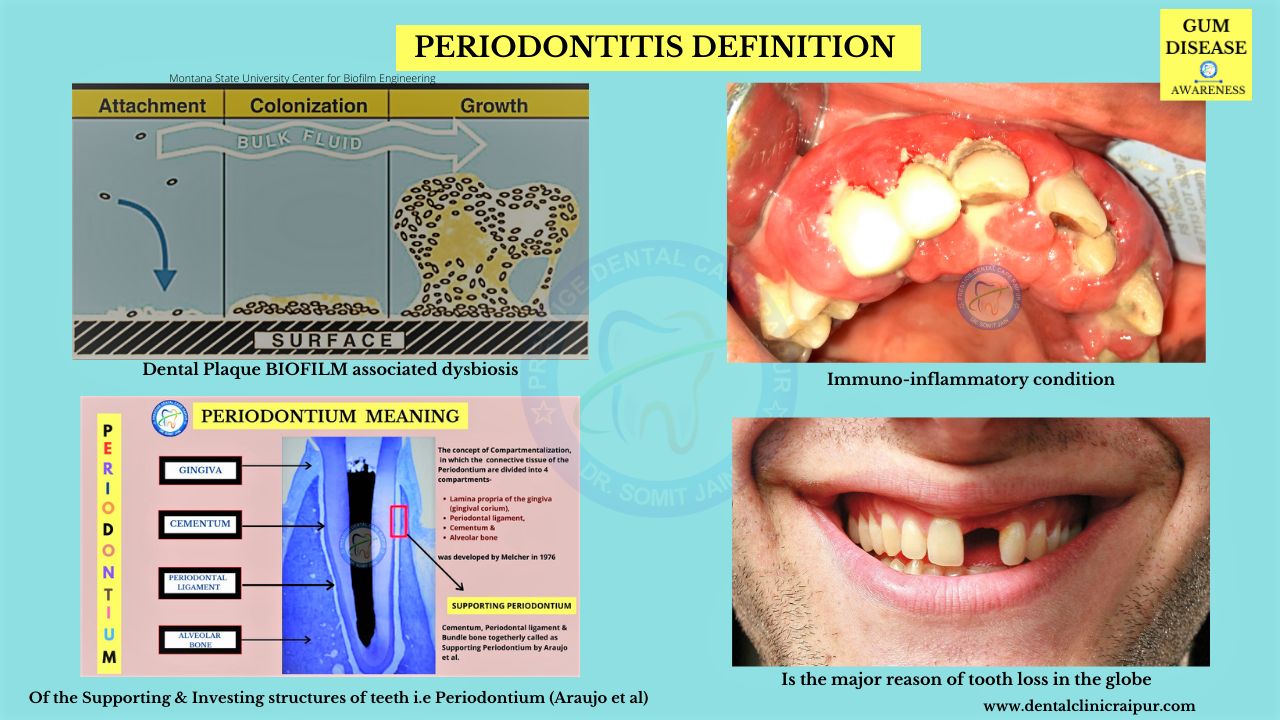
- Periodontal disease/Pyorrhea which is otherwise known as Gum disease around the globe is a collective term used for different conditions affecting one or more tissues in the attachment apparatus of the tooth including gums, cementum, periodontal ligament and the alveolar bone of jaw. The attachment apparatus as a whole is termed as Periodontium.
- Periodontium can be defined as complex supporting and investing structural tissues that holds the teeth in the mouth (Synonym: attachment apparatus of teeth).
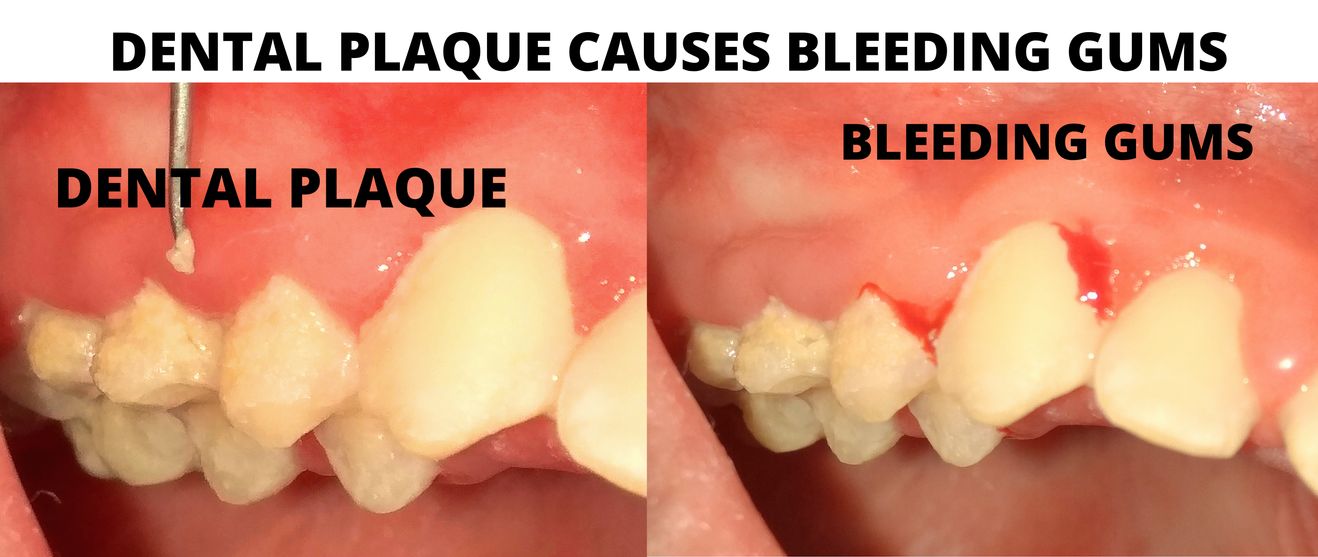
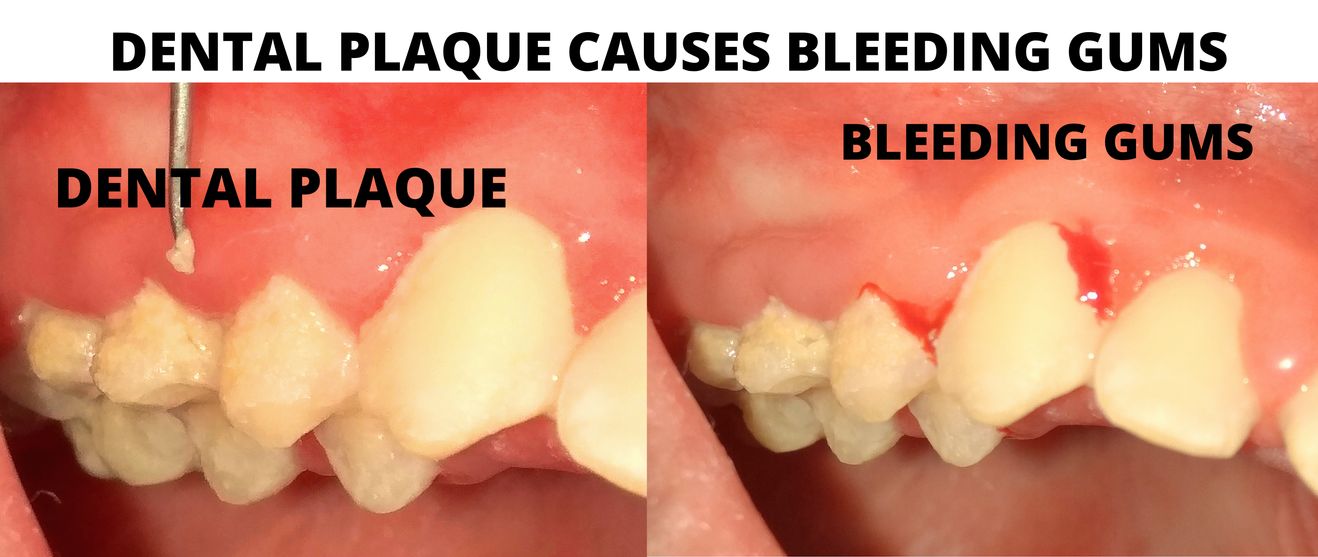
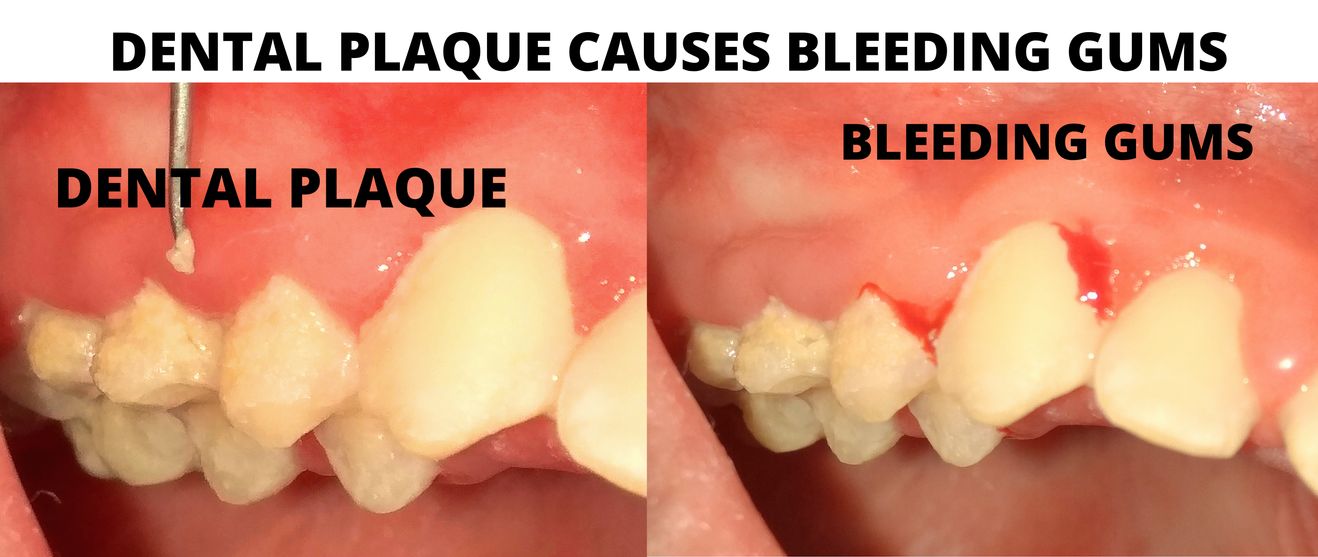
- Dental plaque biofilm is considered to be the most important initiating factor for different forms of periodontal disease.
- The plaque-induced variations of Periodontal disease (Gingivitis & Periodontitis) are extremely prevalent chronic immuno-inflammatory conditions that affect distinct components of the Periodontium including gums and bone.
2#. What is the meaning of Periodontitis ?
PERIODONTITIS DISEASE MEANING:
(Periodontitis que es, Periodontitis definition)
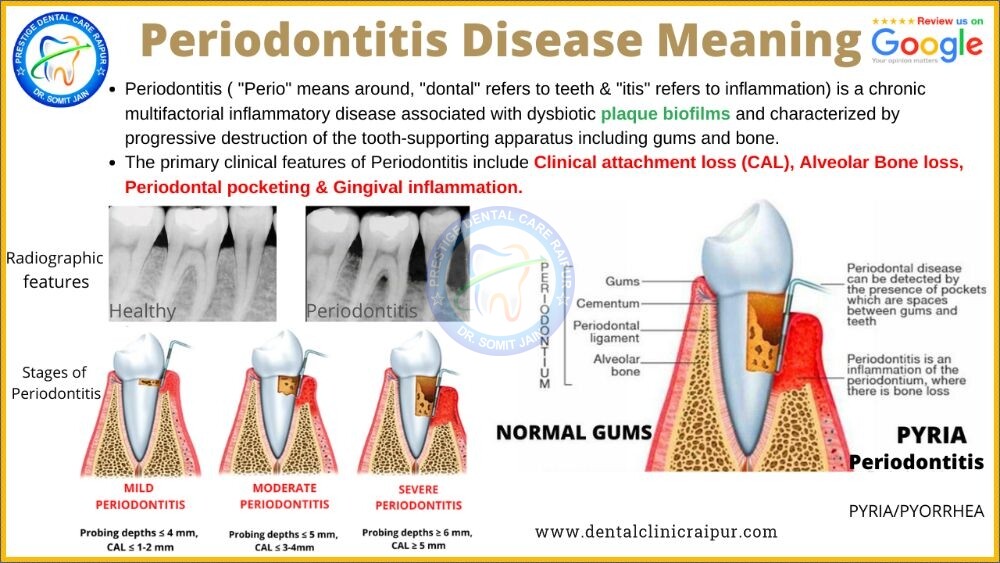
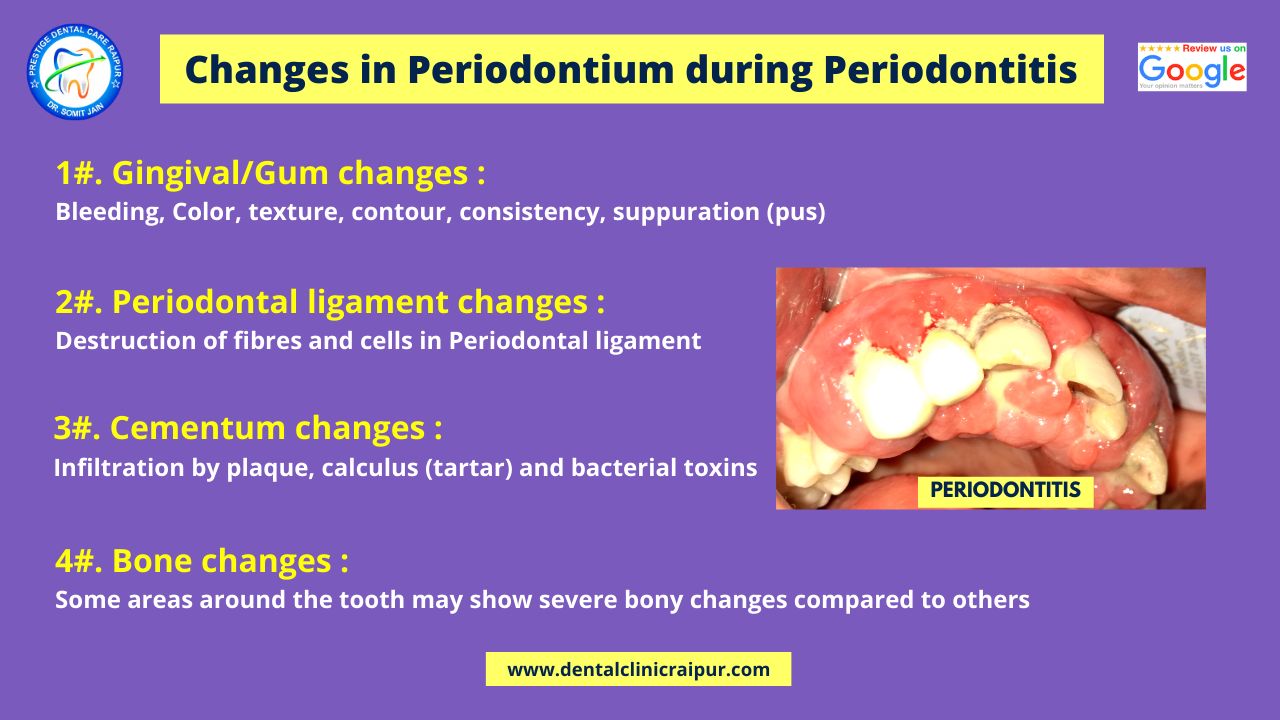
- Periodontitis ( “Perio” generally means around, “dontal” signifies teeth & “itis” as we all know is inflammation) is a chronic multifactorial immuno-inflammatory disease associated with plaque biofilms (dysbiotic in nature) and may proceed to destruction of the tooth‐supporting periodontium including gums and bone.
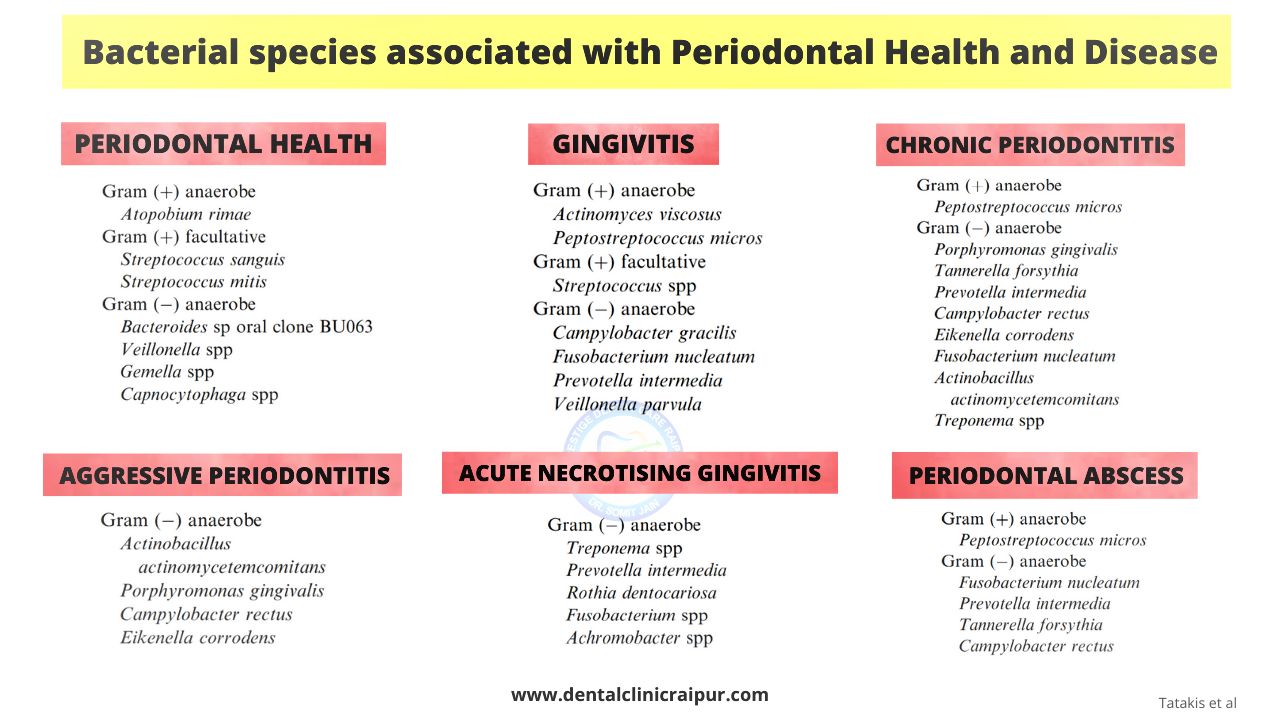
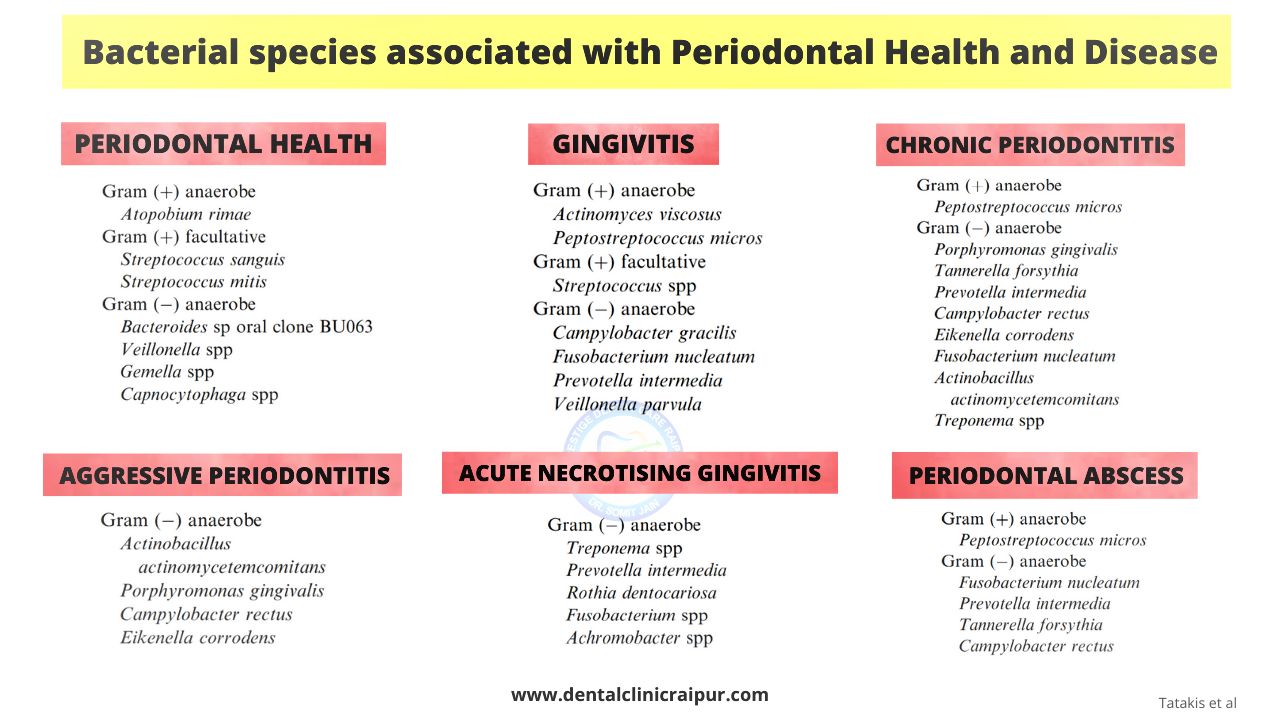
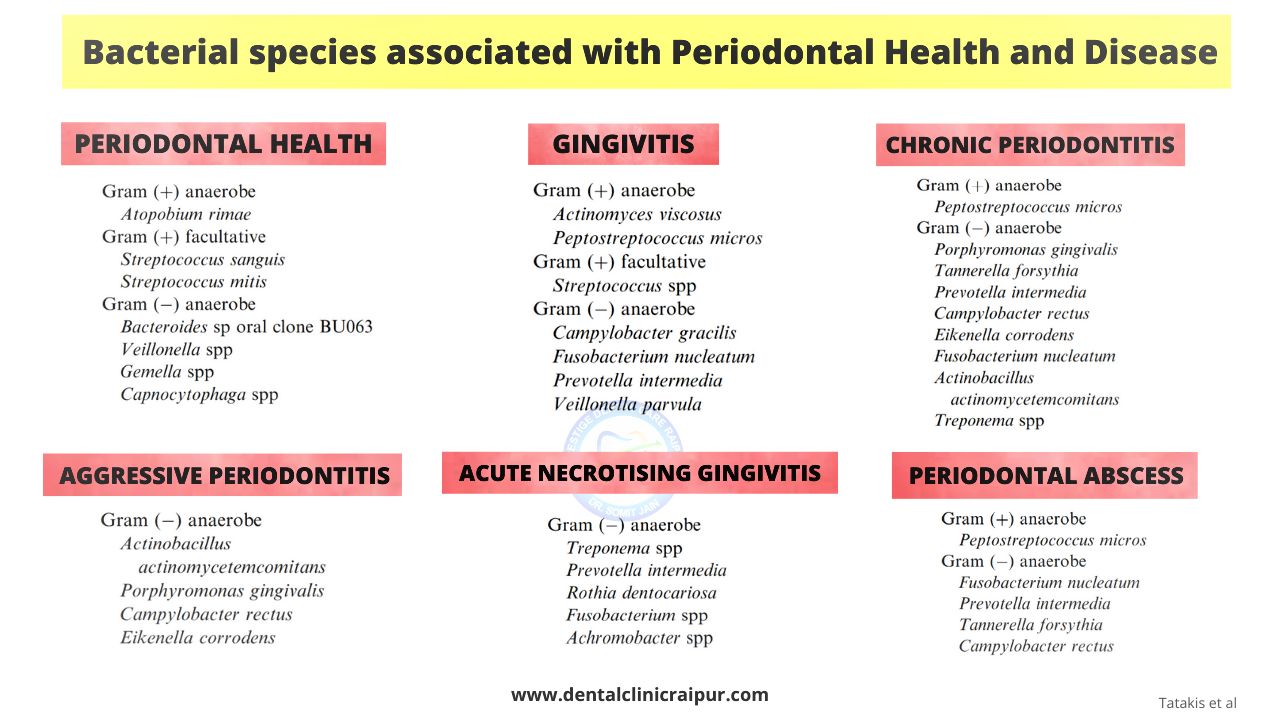
- The most harmful and tissue invasive pathogen which has been seen to be associated with gum/periodontal diseases are primarily Gram negative anaerobic bacteria and may include A.actinomycetemcomitans, Porphyromonas gingivalis & Prevotella intermedia.
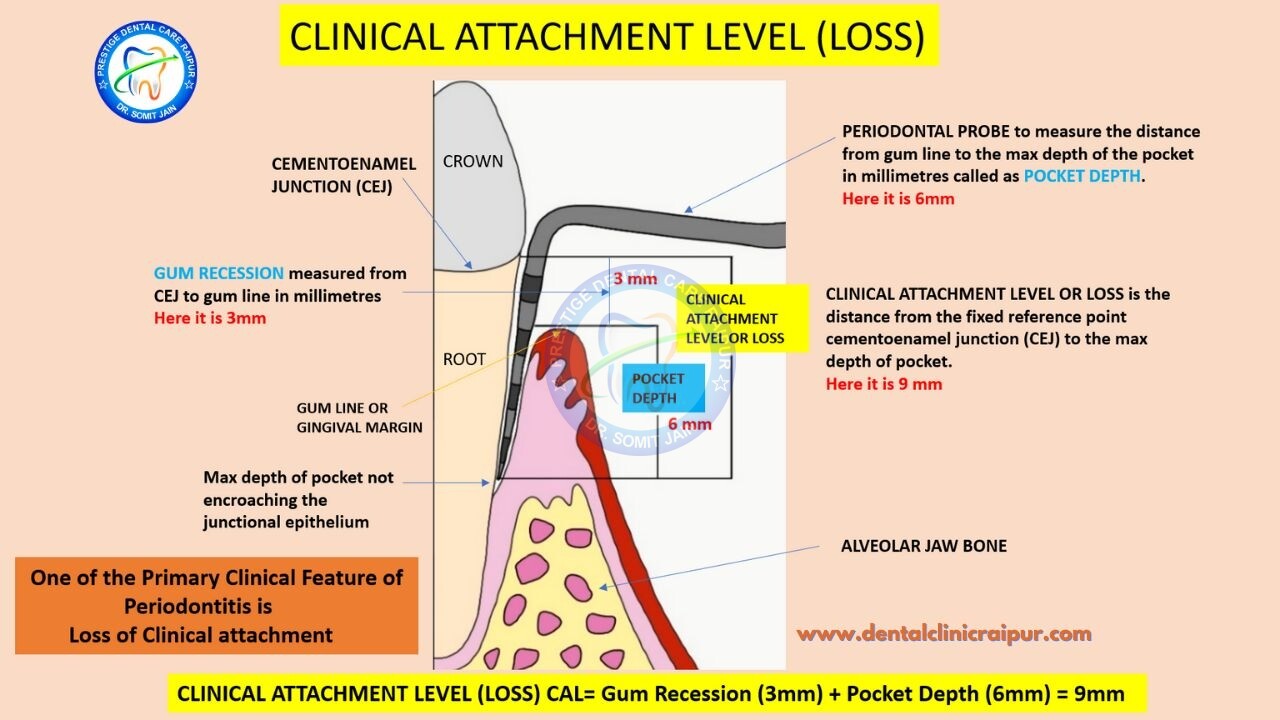
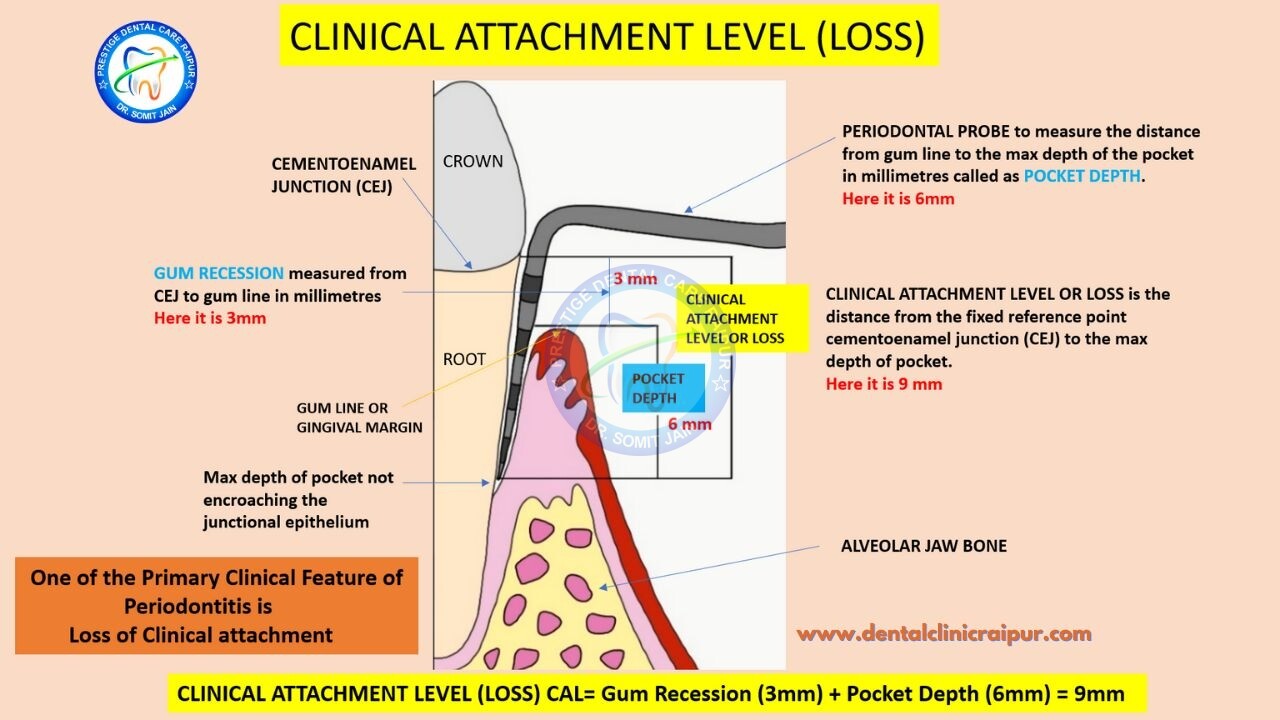
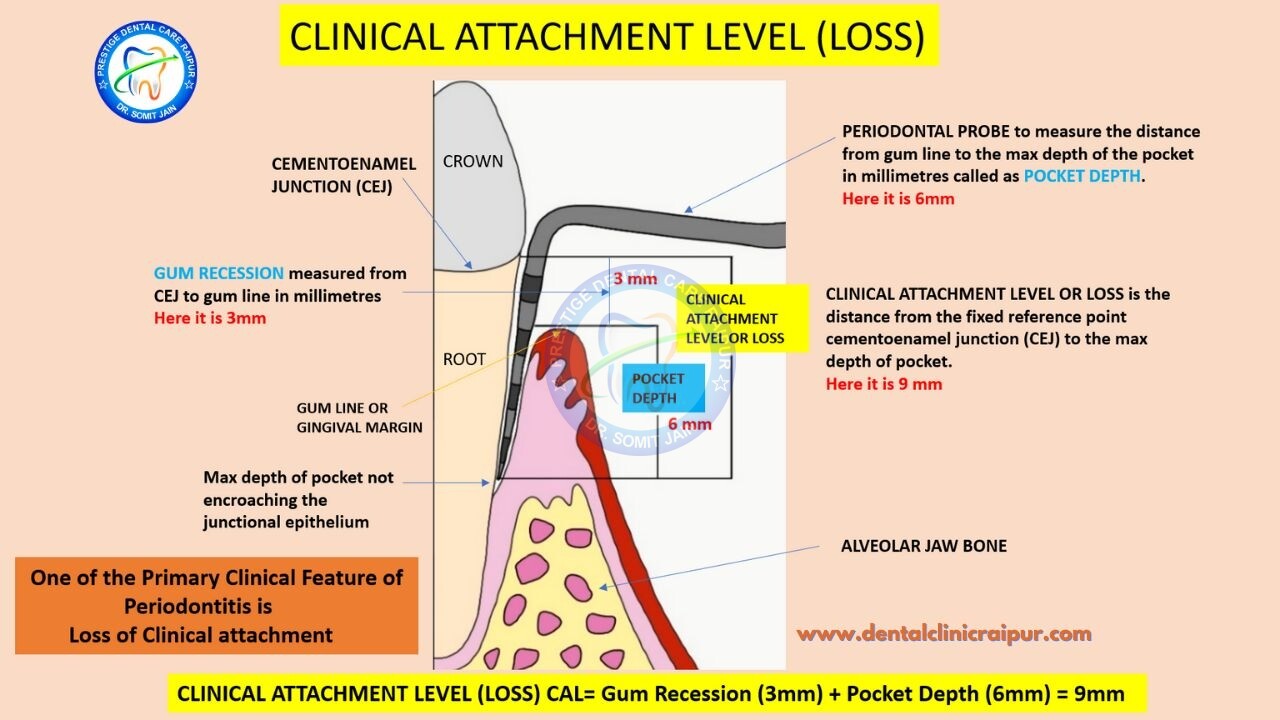
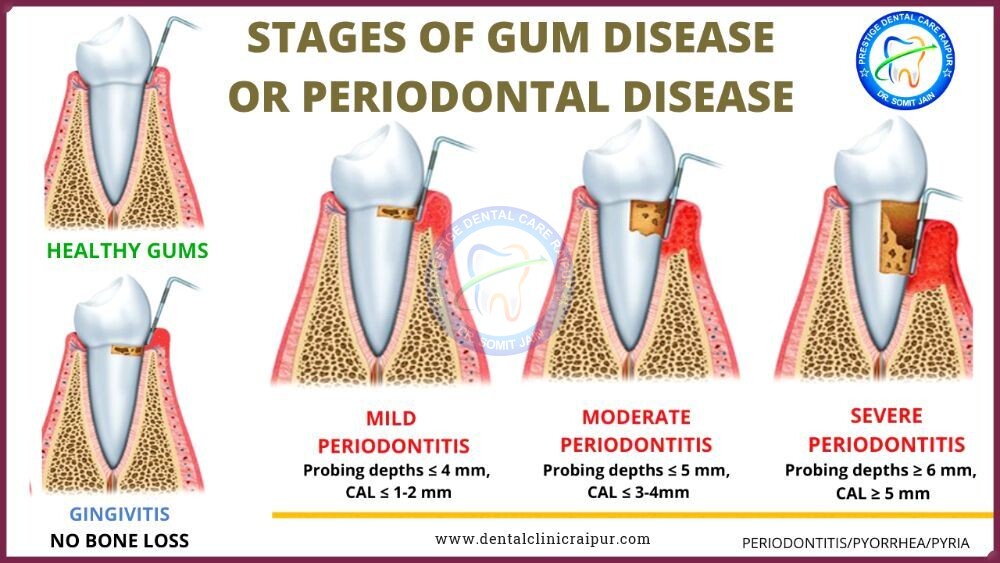
- The principal clinical features of Periodontitis include Loss of Clinical Periodontal attachment (CAL), jaw Bone loss, increase in pocket depth & Gum inflammation.
- Other names : Gum disease, Periodontal disease, Pyorrhea, Pyria, पायरिया
- Specialty: Dentistry
- Symptoms: Bleeding and swollen gums, bad breath, gums pulling away from teeth, loose teeth.
- Causes: Primarily by the harmful bacteria present in dental plaque biofilm.
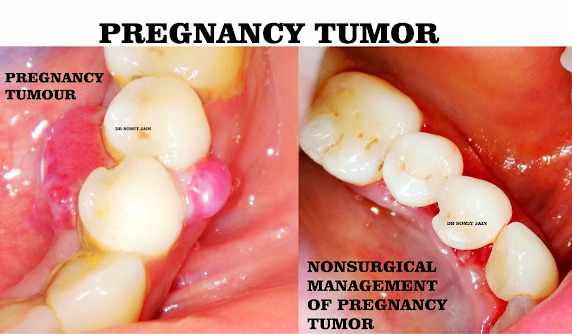
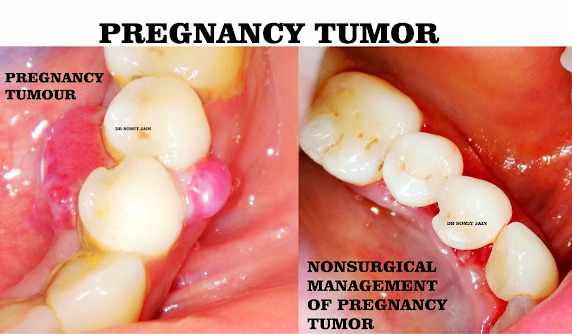
- Risk Factors: Diabetes, Smoking, Hormonal imbalances
- Diagnostic Criteria: Thorough Clinical, Radiographic and Occlusal examination (OPG, Bitewing X-rays)
- Treatment: Regular professional cleaning, Non-surgical & Surgical Periodontal therapy, Home remedies.
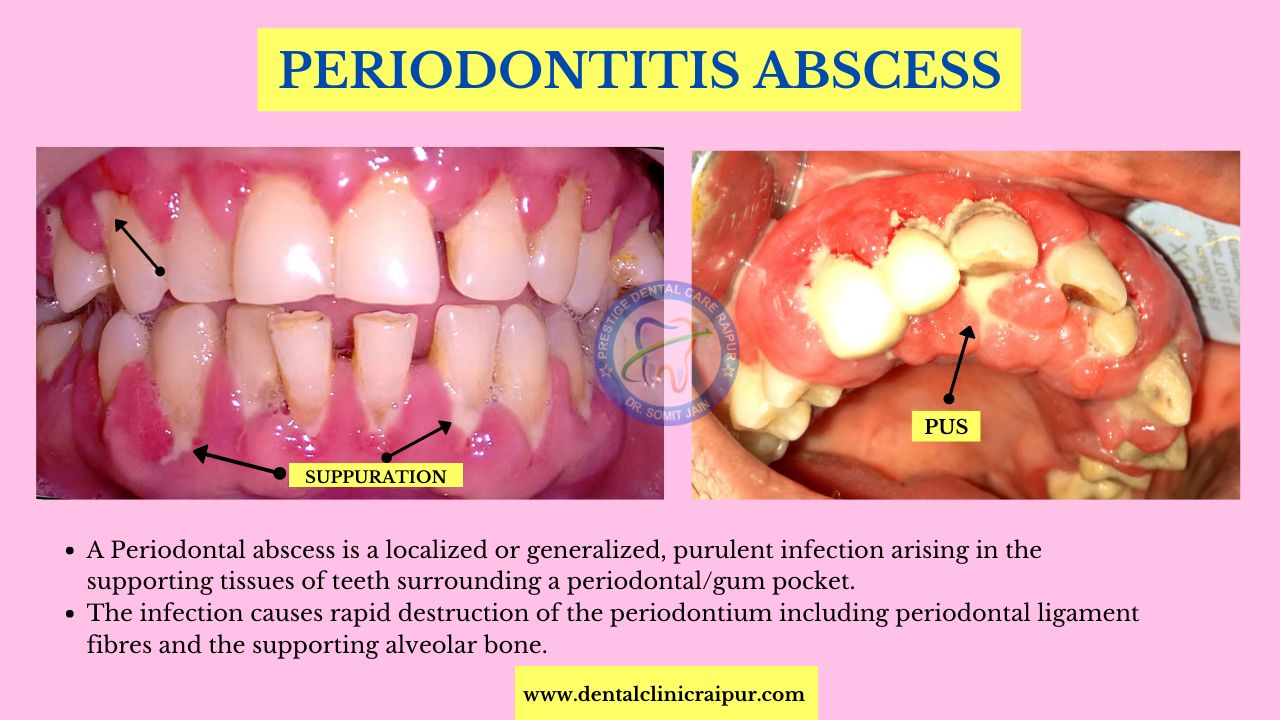
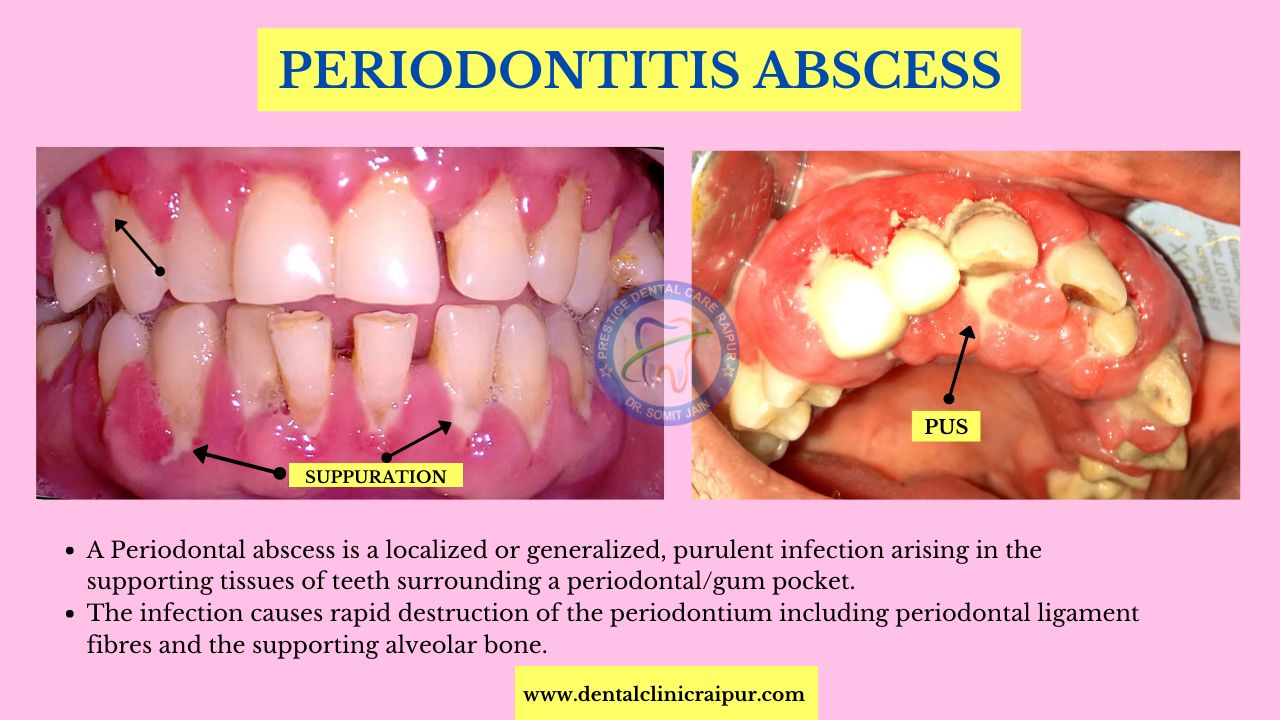
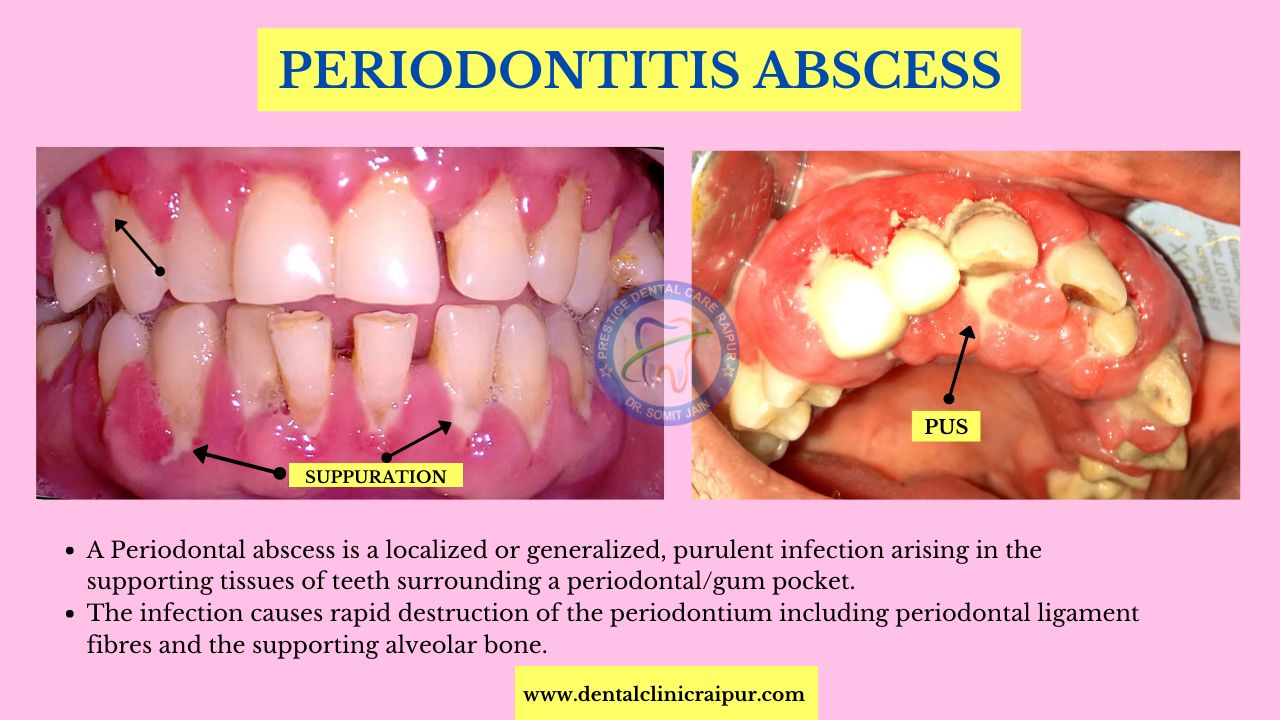
- Complications: Periodontal abscess, tooth loss, systemic complication in severe inflammatory cases.
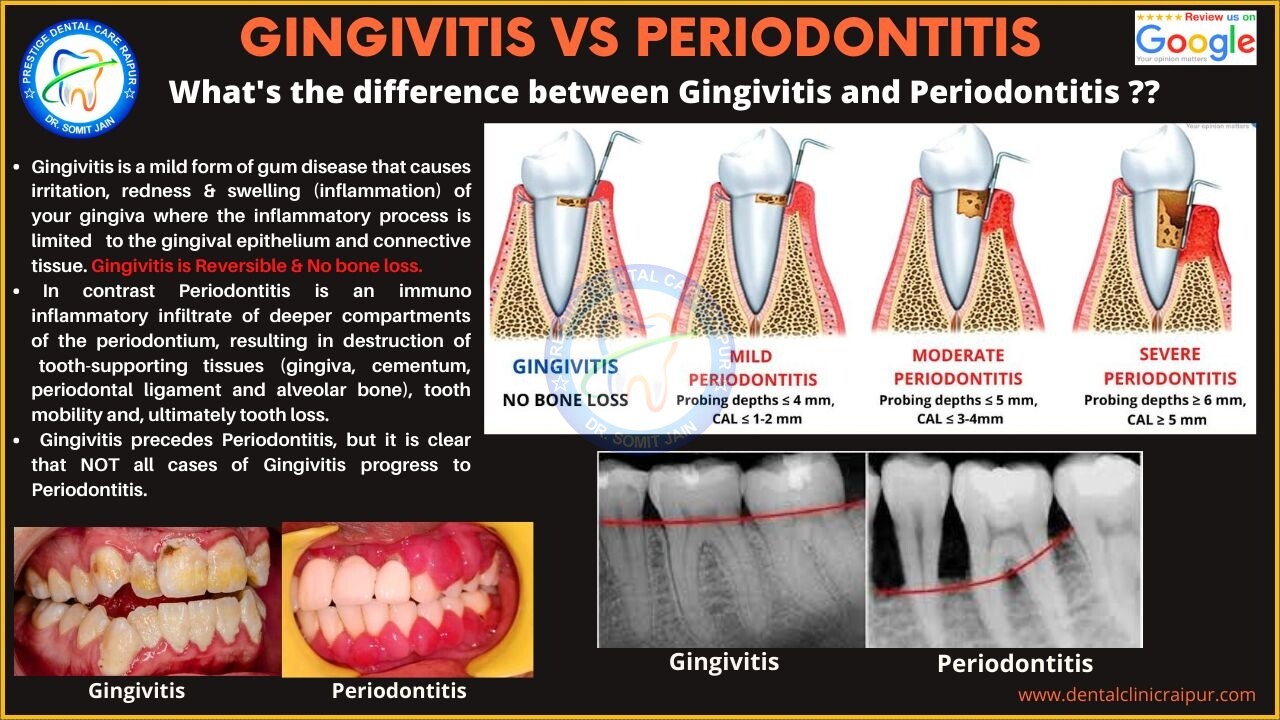
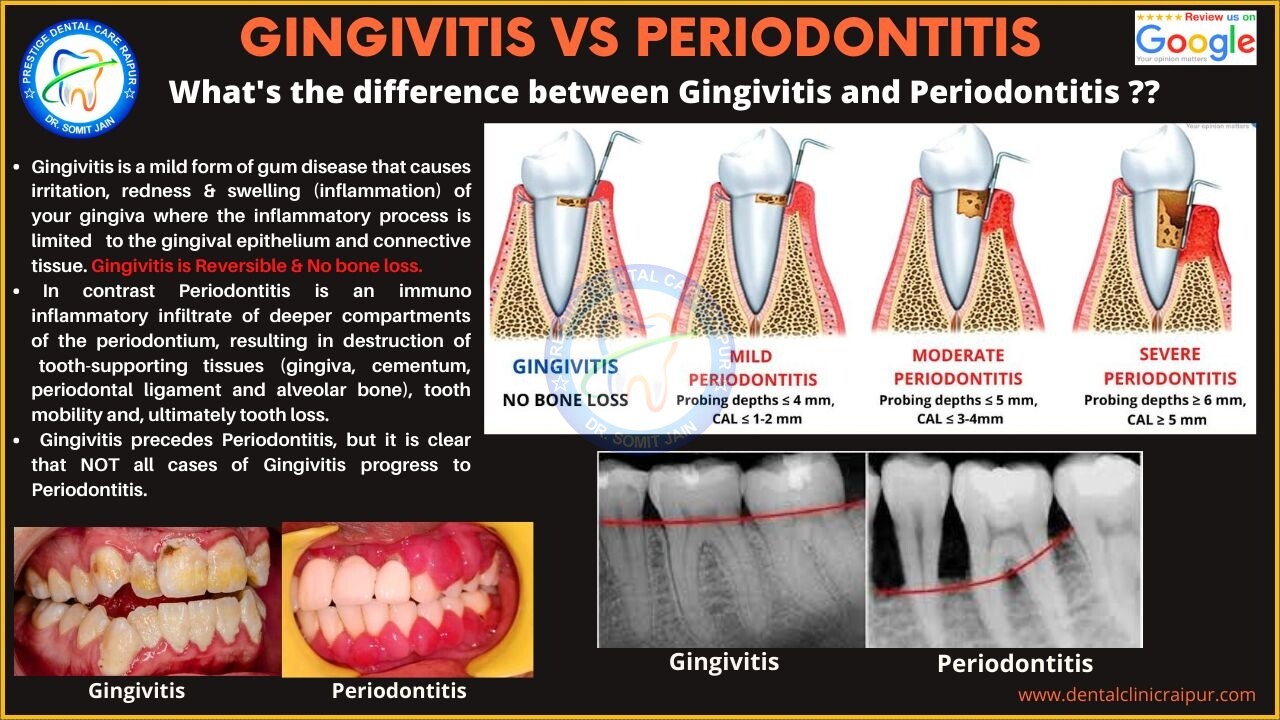
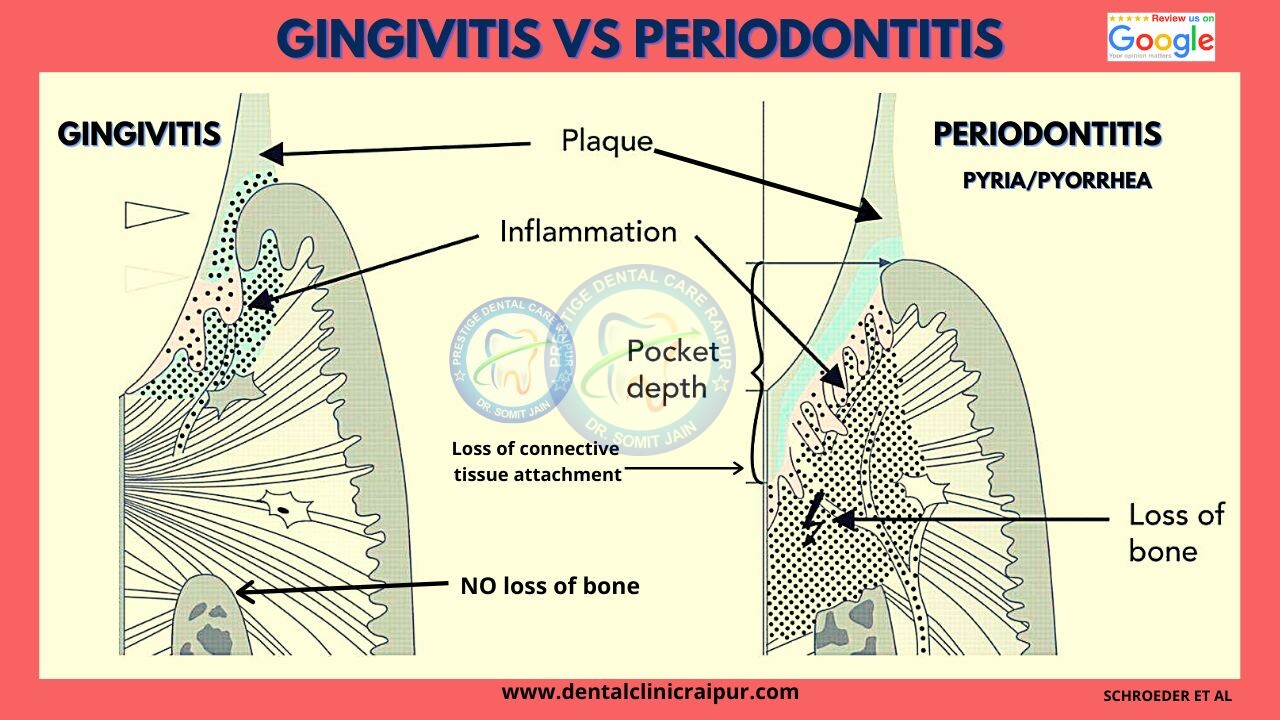
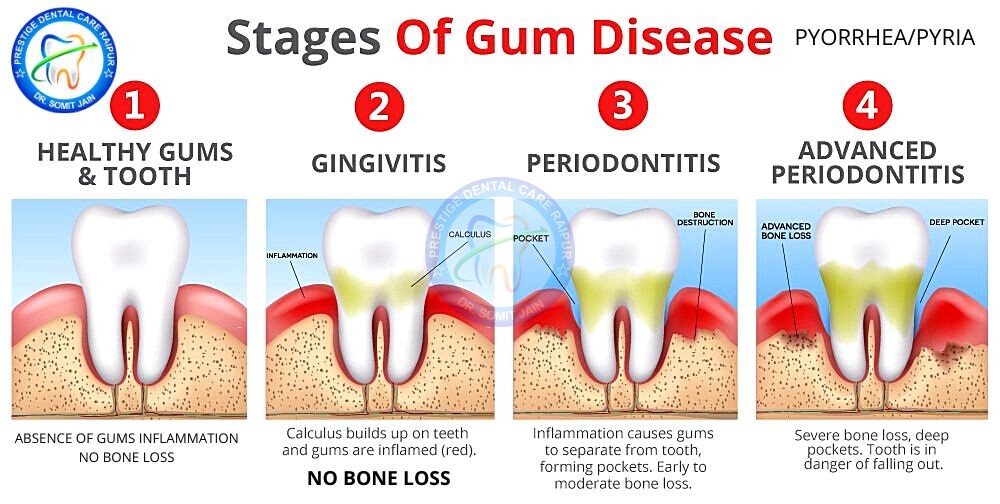
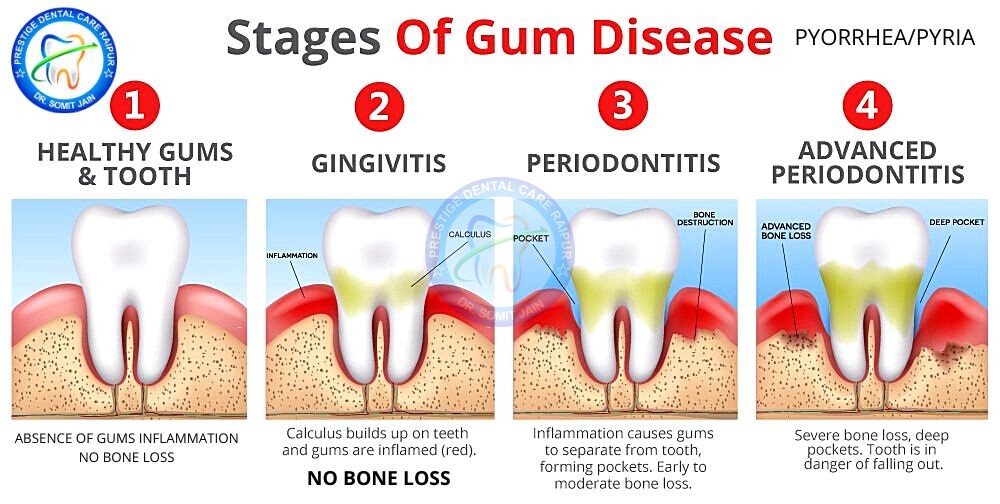
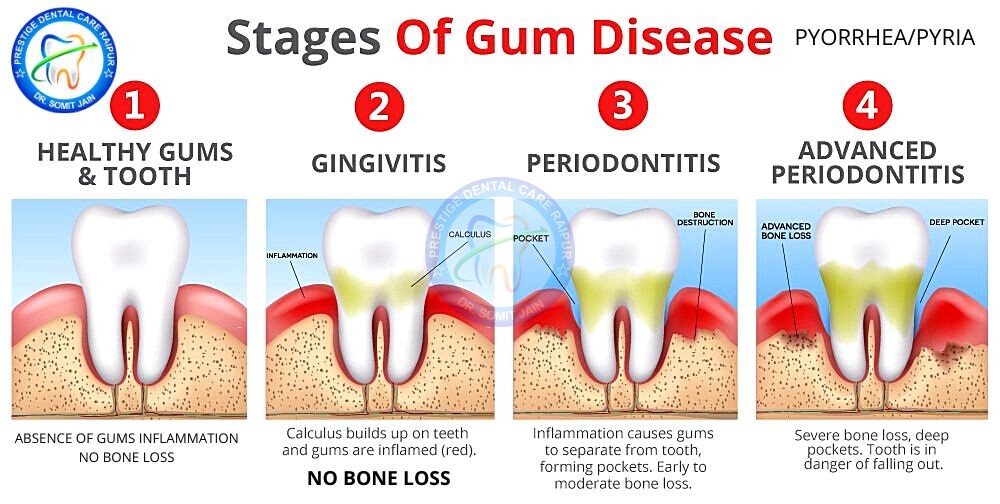
3#. What is the difference between Gingivitis and Periodontitis?
Gingivitis Vs Periodontitis
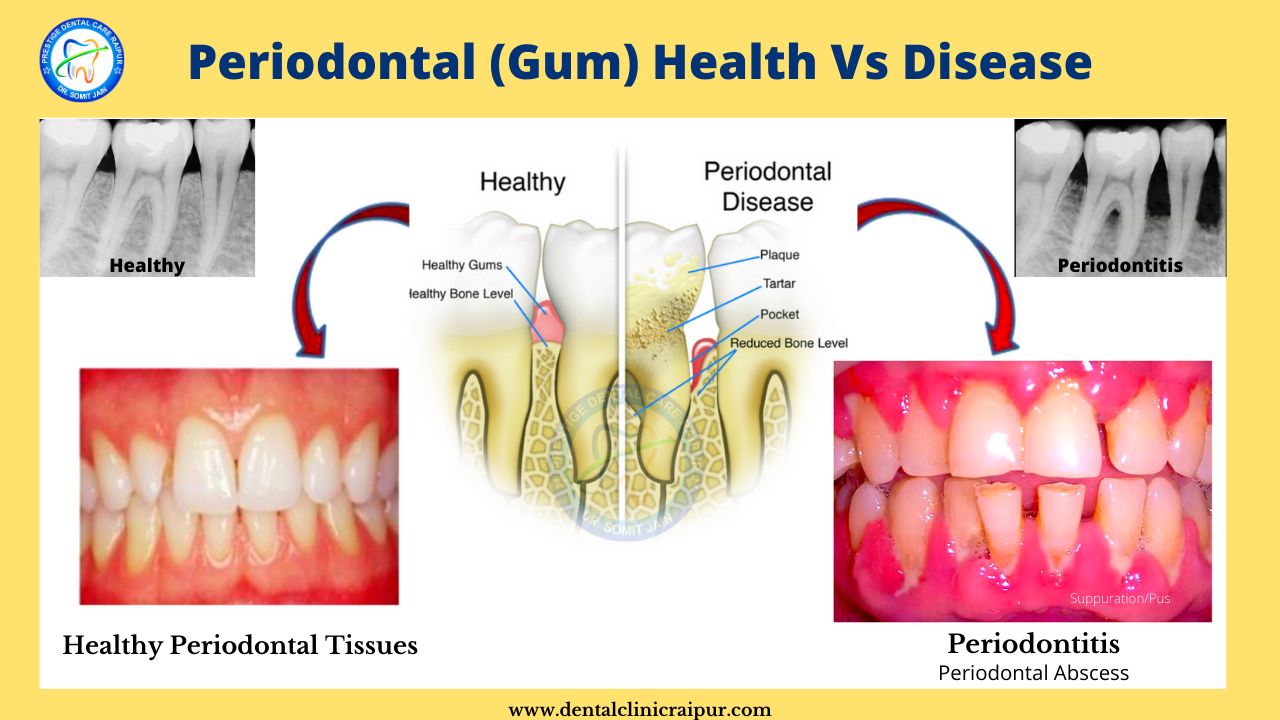
- Gingivitis and Periodontitis are both types of Periodontal disease or Gum disease.
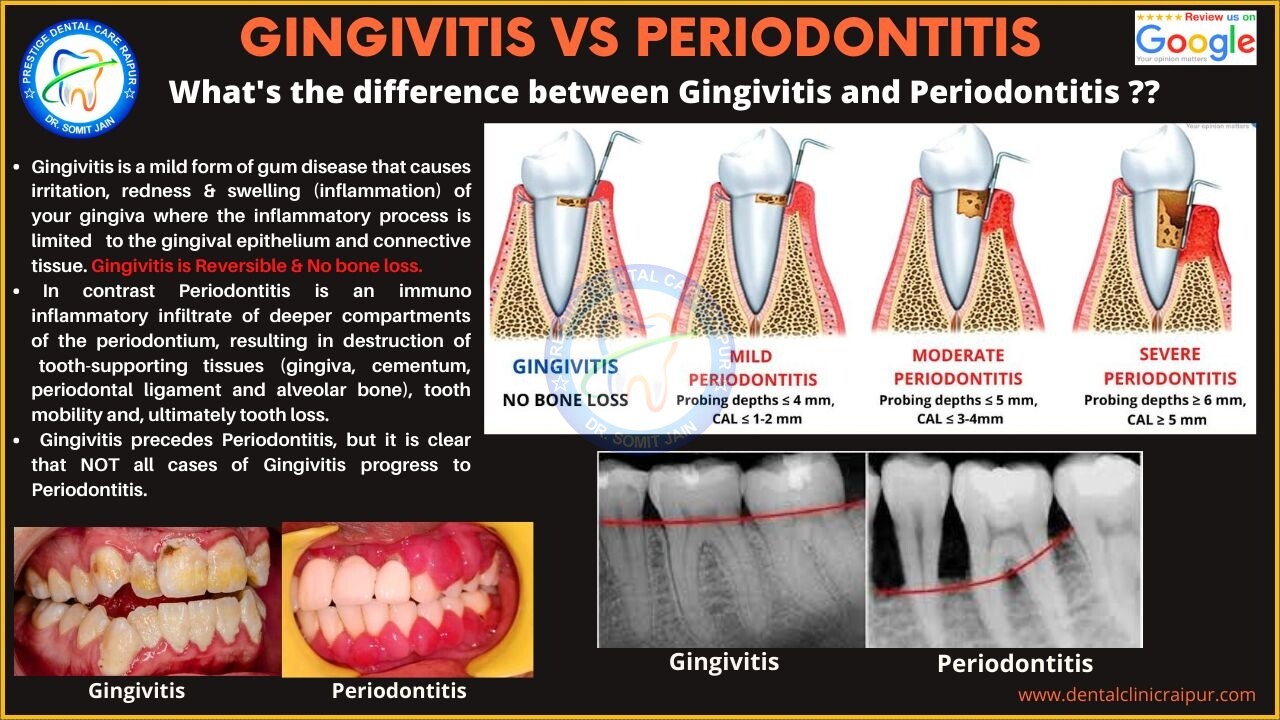
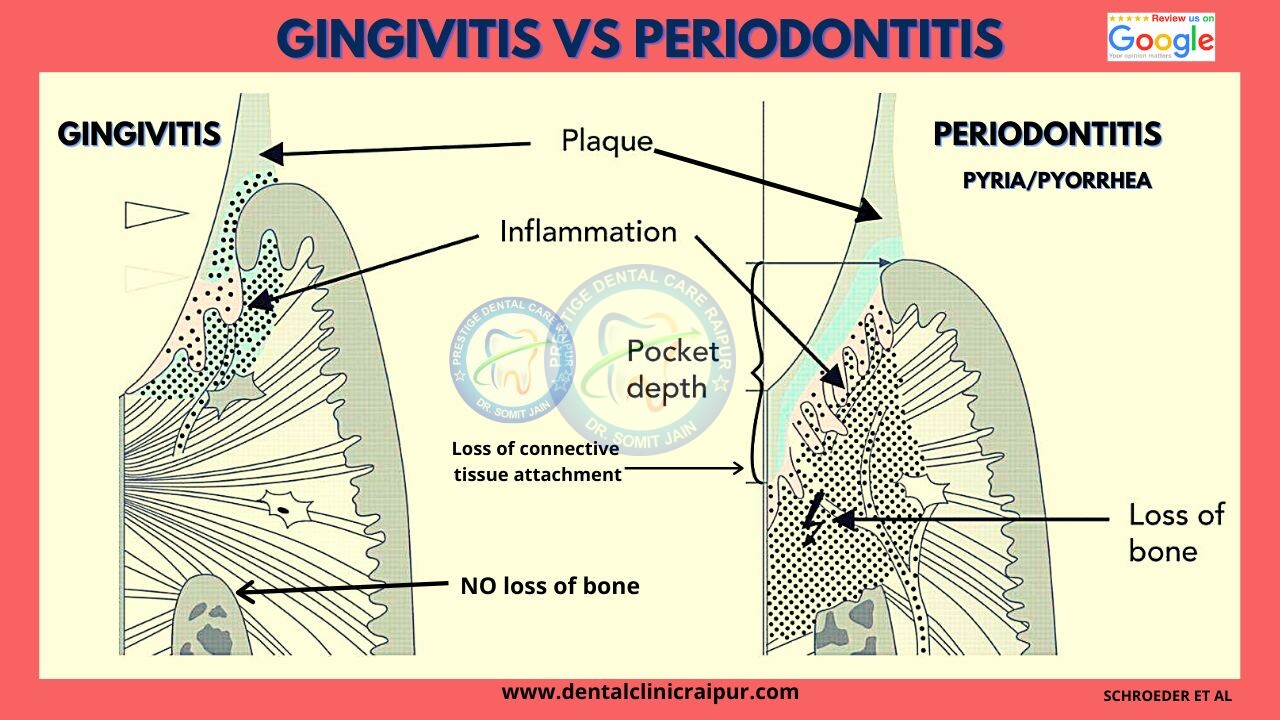
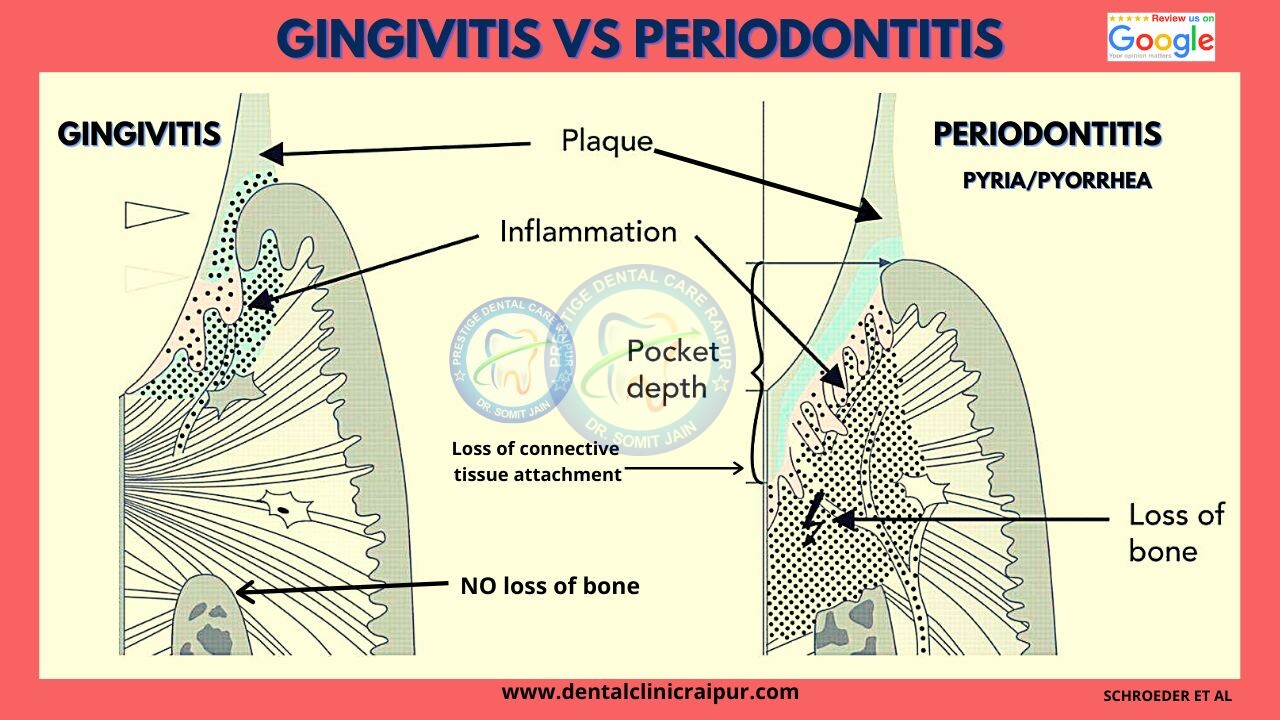
- Gingivitis is a mild form of Periodontal disease that causes irritation, redness & swelling (inflammation) of your gingiva/gums where the inflammatory process is limited to the gingival epithelium and connective tissue. Gingivitis is Reversible & No bone loss.
- In contrast Periodontitis is an immuno inflammatory infiltrate of deeper compartments of the periodontium, resulting in destruction of tooth-supporting tissues including gingiva, cementum, periodontal ligament and alveolar bone (Periodontitis is NOT reversible because it involves bone loss, which cannot be recovered), tooth mobility and, ultimately tooth loss.
- Gingivitis may lead to Periodontitis, but it is clear that NOT all cases of Gingivitis proceed to Periodontitis.
4#. What is the meaning of the term "Periodontist" or "Gum Specialist"
Periodontist Meaning
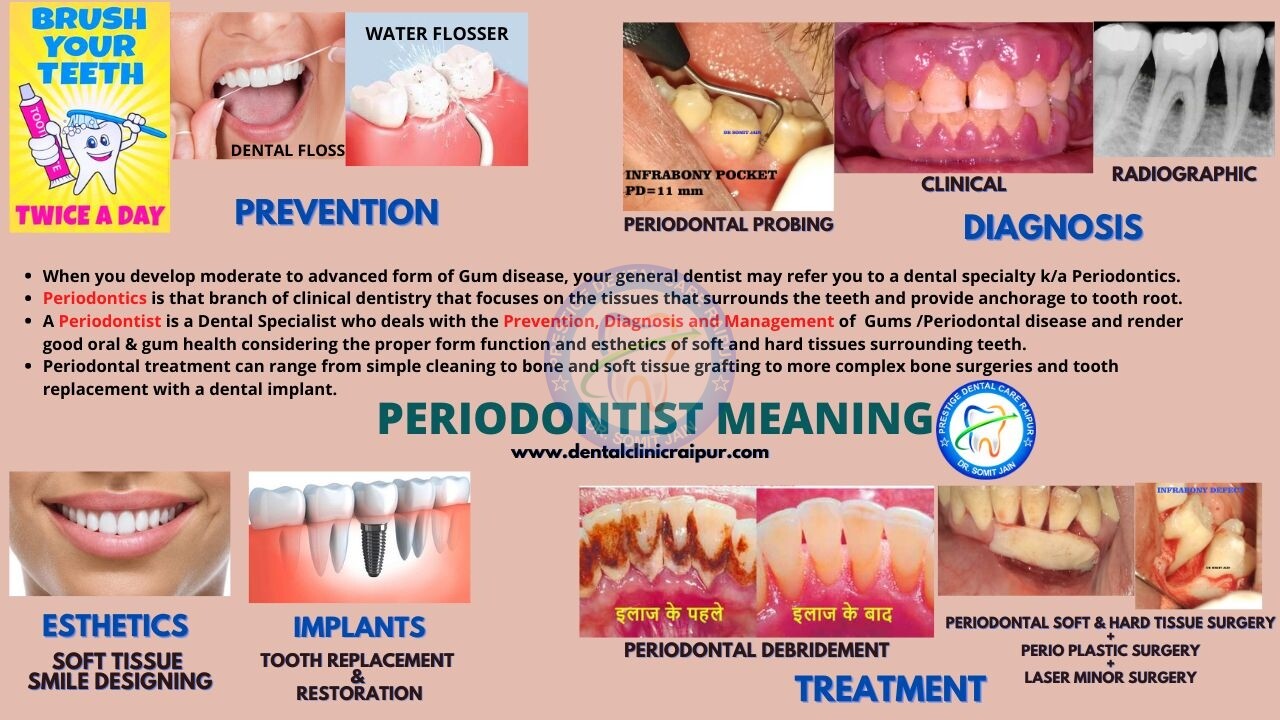
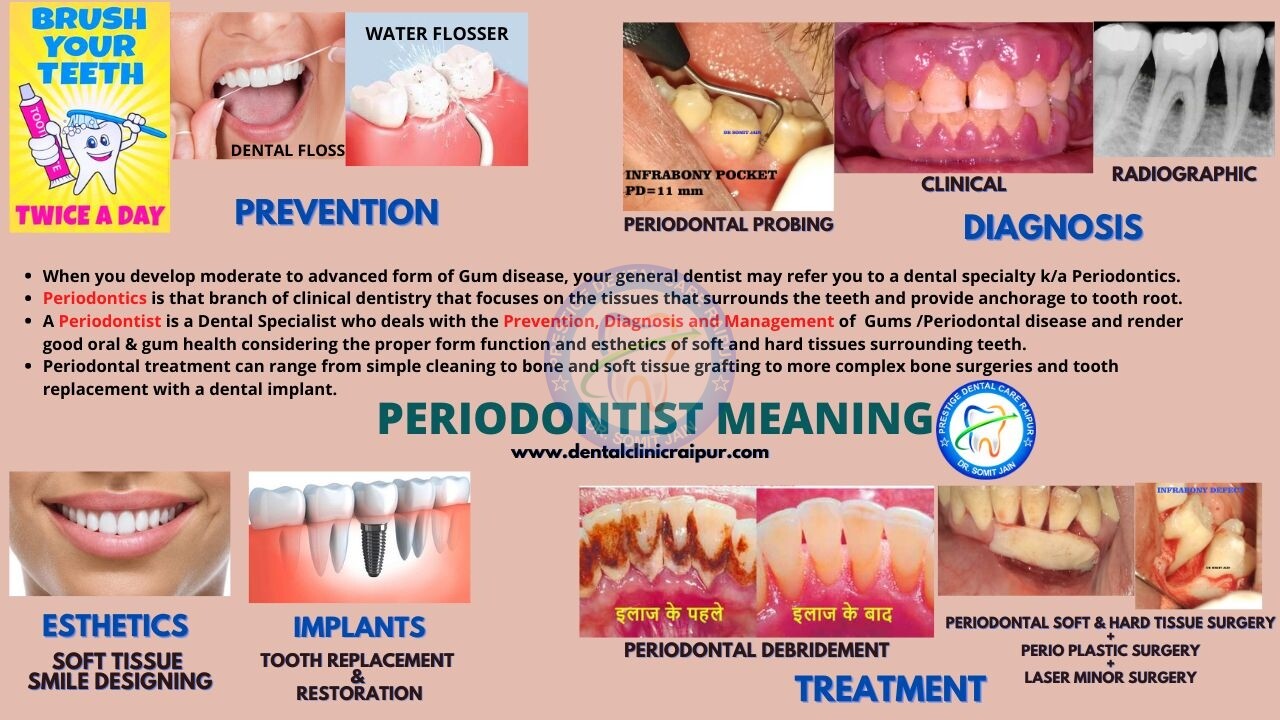
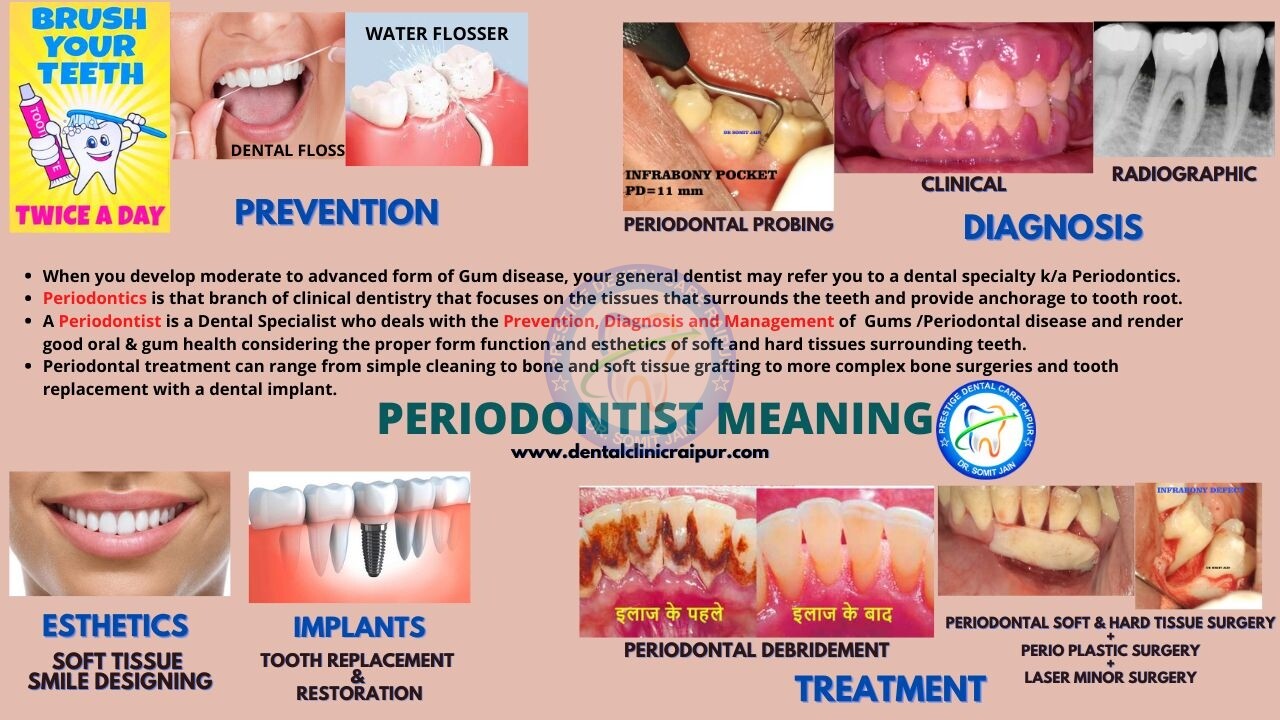
- When you develop moderate to advanced form of Gum disease, your general dentist may refer you to a dental specialty k/a Periodontics.
- Periodontics is that branch of clinical dentistry that focuses on the tissues that surrounds the teeth and provide anchorage to tooth root.
- A Periodontist is a Dental Specialist who deals with the Prevention, Diagnosis and Management of Gums /Periodontal disease and render good oral & gum health considering the proper form function and esthetics of soft and hard tissues surrounding teeth.
- Periodontal treatment can range from simple cleaning to bone and soft tissue grafting to more complex bone surgeries and tooth replacement with a dental implant.
5#. What do you understand by the term Periodontium?
Periodontium
- The Dental Unit is an organ consisting of the Teeth and Periodontium (teeth supporting hard and soft tissues). Dental Unit plays a key role in deglutition, phonation, proprioception, support for facial musculature and Temporomandibular joint (TMJ) & maintenance of a general sense of well being.
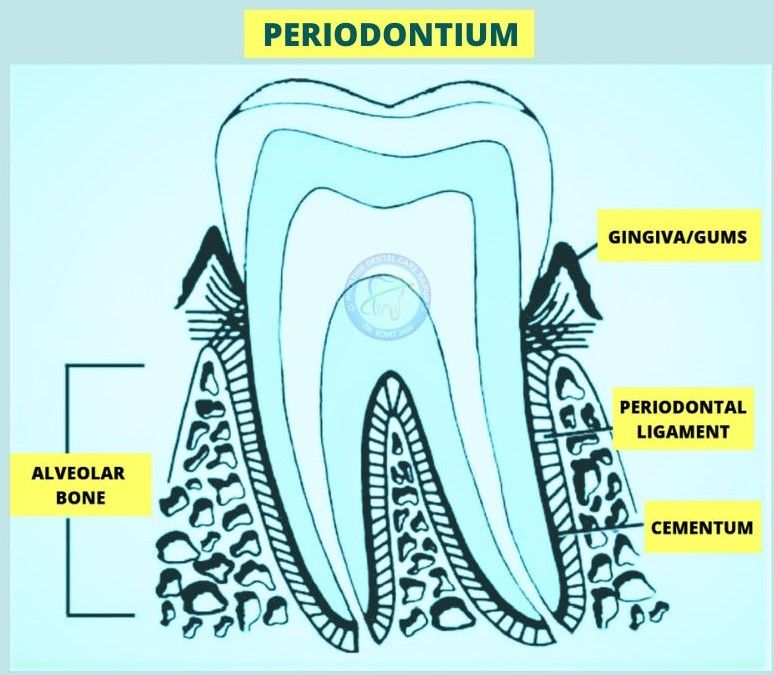
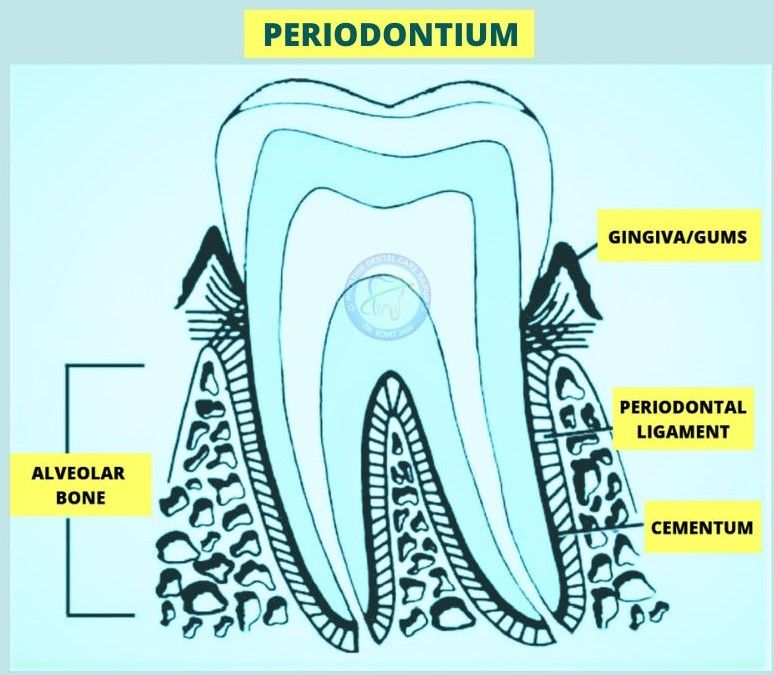
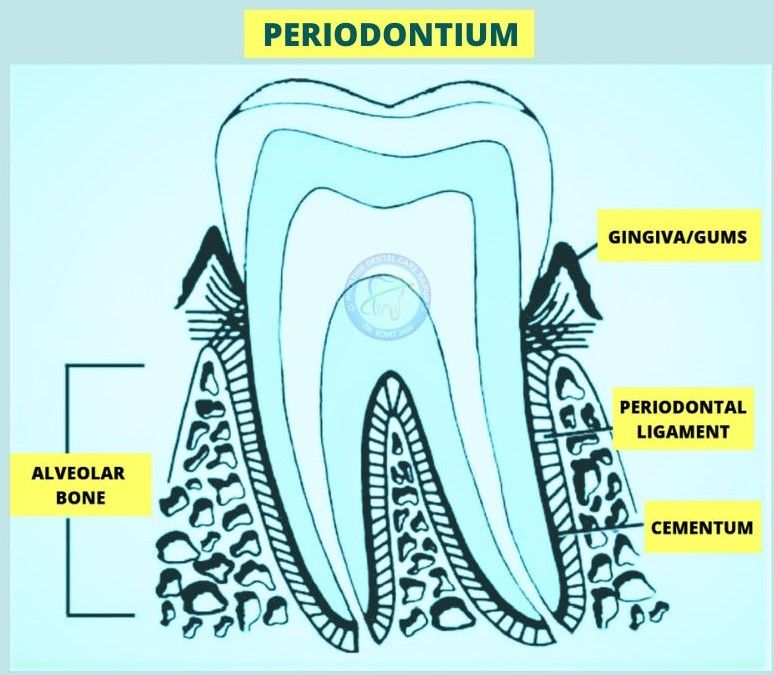
- Supporting tissues of the teeth known collectively as the Periodontium (from the Greek peri, around, and odontos, a tooth) includes various tissue compartments which anchor the teeth to the jaw bone.
- Periodontium comprises of four different tissue compartments Lamina propria of gingiva, root cementum, periodontal ligament and Bundle bone (Alveolar bone proper).
- Provide interdental connection among the row of teeth.
- Tissue compartments also provide a protective seal for the mucosal openings created by erupting teeth via the junctional epithelium and hemidesmosomes to withstand the masticatory forces and to defend the sulcular space between the teeth and soft tissue from the foreign invaders (microorganisms).
- These tissue compartments behave biologically developmentally and functionally as a protective unit for the teeth.
Functions of Periodontium (Schroeder et al)
- Attachment : Attach the teeth to their bony housing and to one another.
- Resistance : Resist and resolve the forces generated by mastication, speech and deglutition.
- Protective Seal : Maintain the integrity of the body surface by separating the internal and the external environment.
- Balance : Adjust for structural changes associated with wear & secondary eruption and ageing through continuous regeneration and remodeling.
- Defense: Defend against the noxious external environment influences that are present in the oral cavity.
Supporting Periodontium/Attachment apparatus – Consists of root cementum, the periodontal ligament, and the alveolar bone (proper).
Alveolar bone proper – Bony wall of the alveolus, comprising a relatively thin perforated plate adjacent to the root (see Lamina dura). It consists of cancellous bone (with Sharpey’s fibers forming bundle bone), except where the socket involves lamellated bone as part of the cortical plate. It is a portion of the alveolar process.
Bundle bone – That portion or entity of alveolar bone proper in which the principal fibers of the periodontal ligament are anchored.
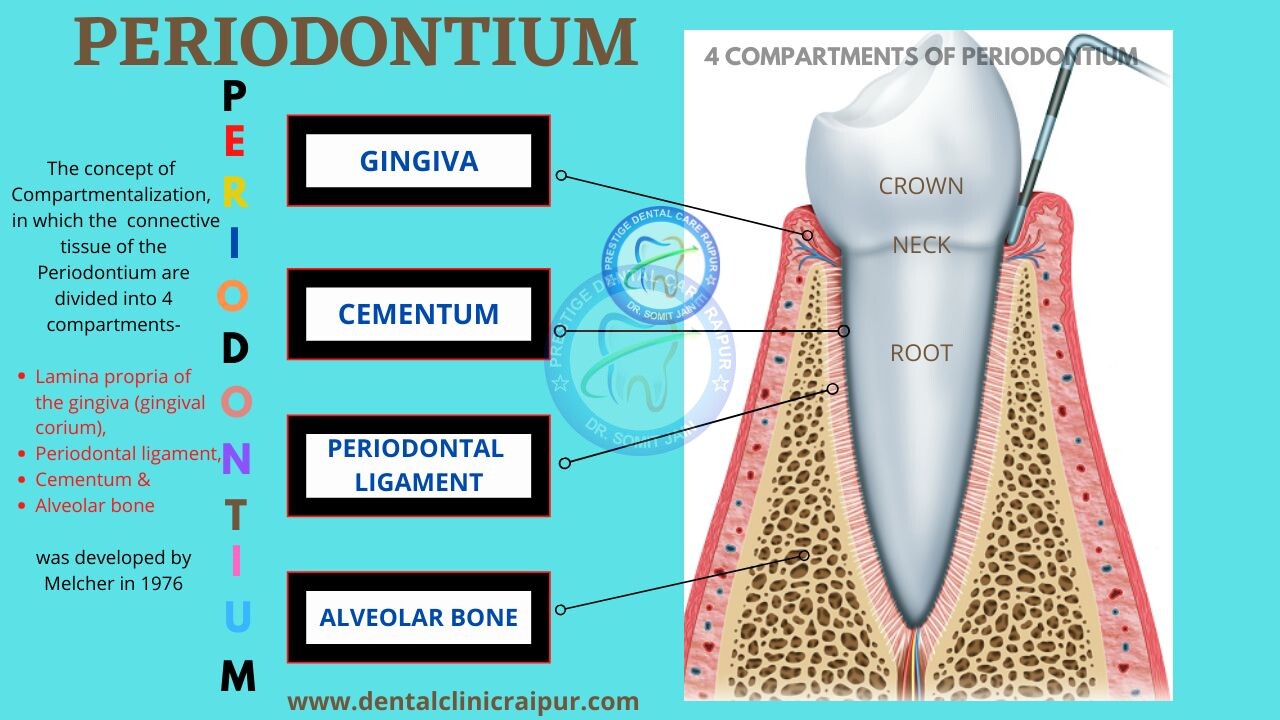
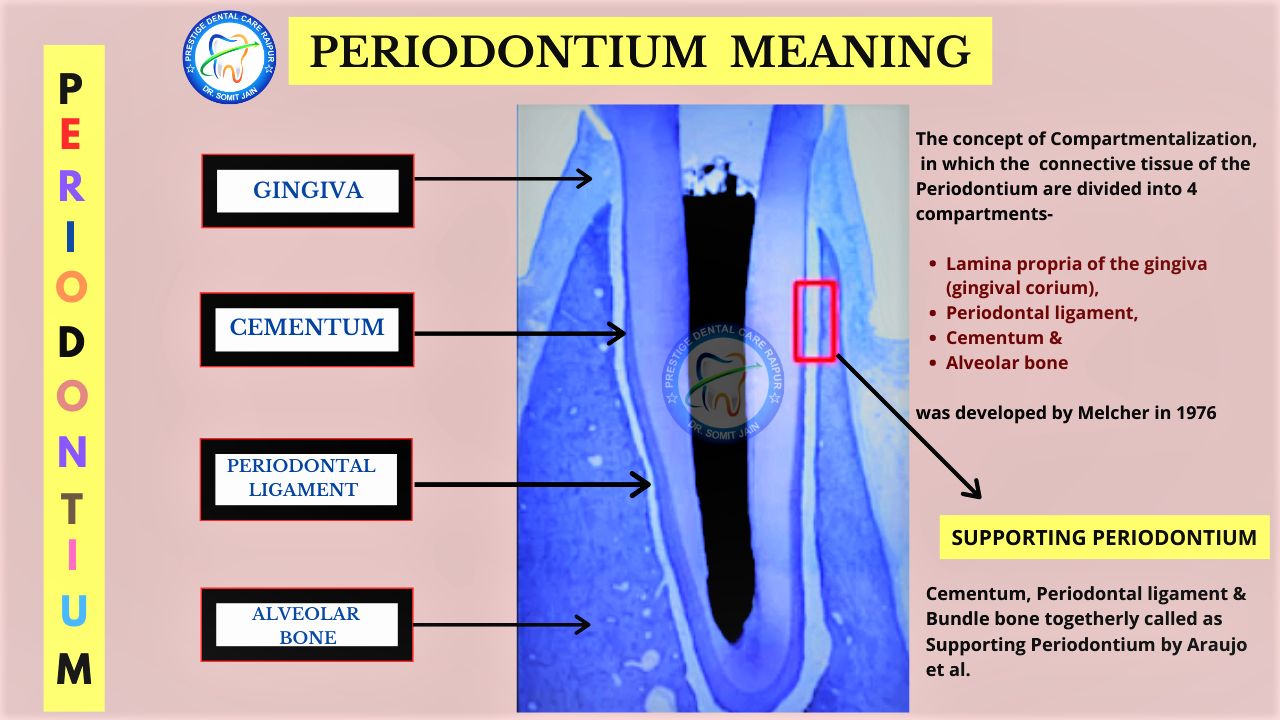
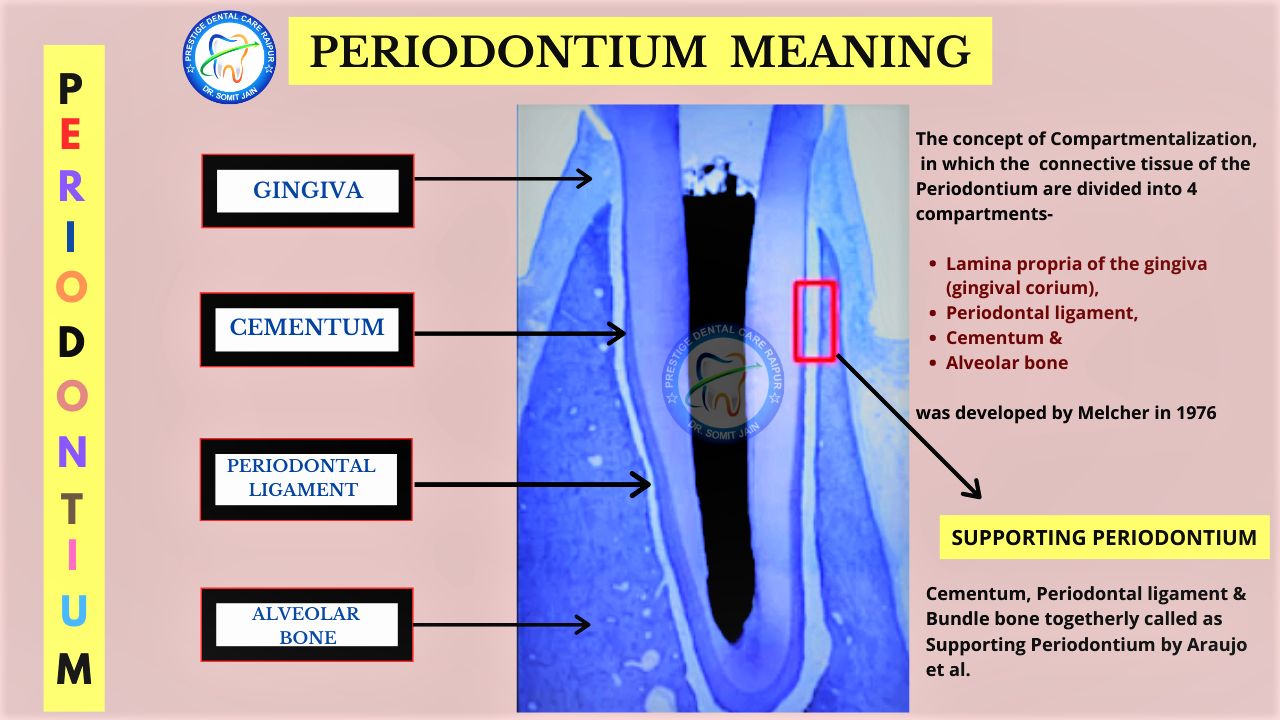
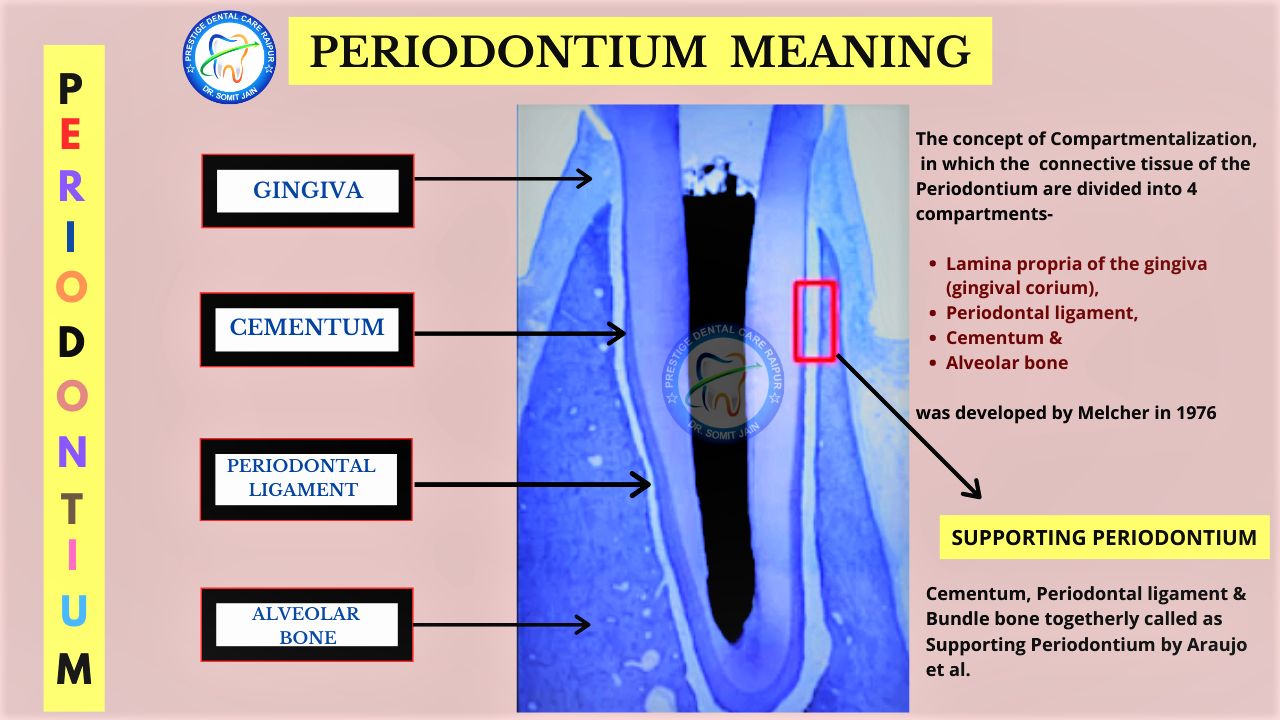
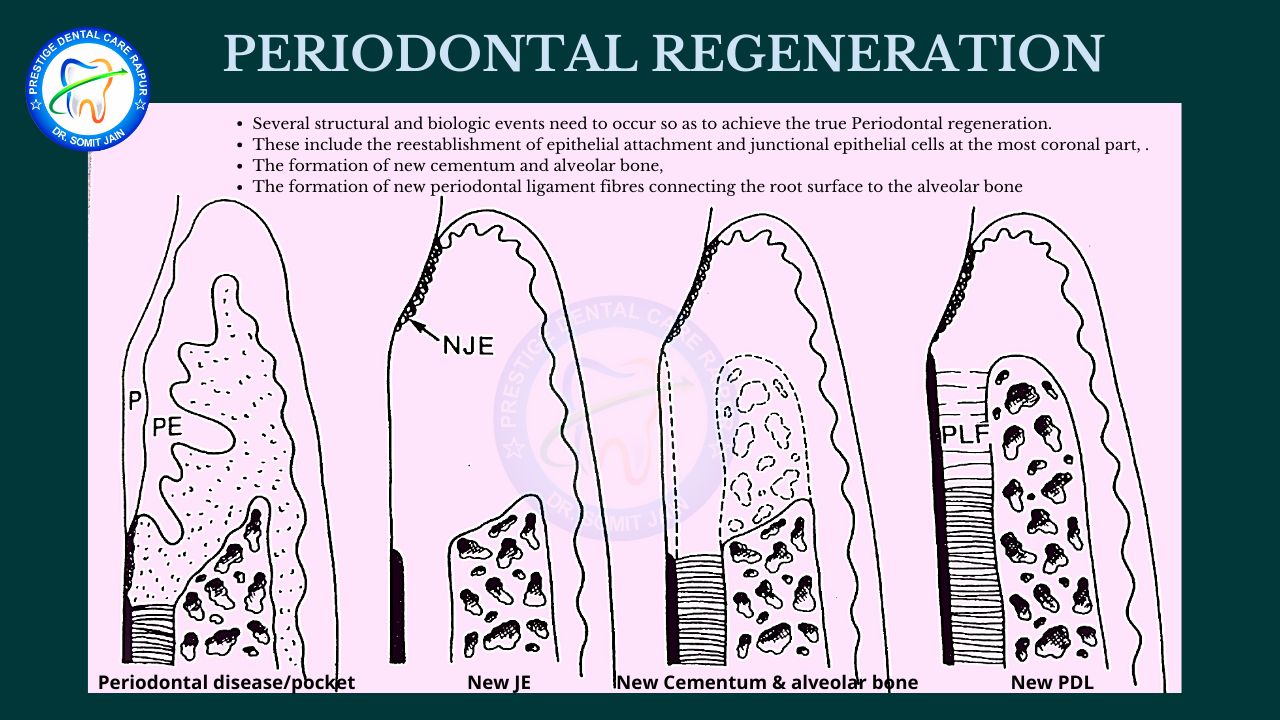
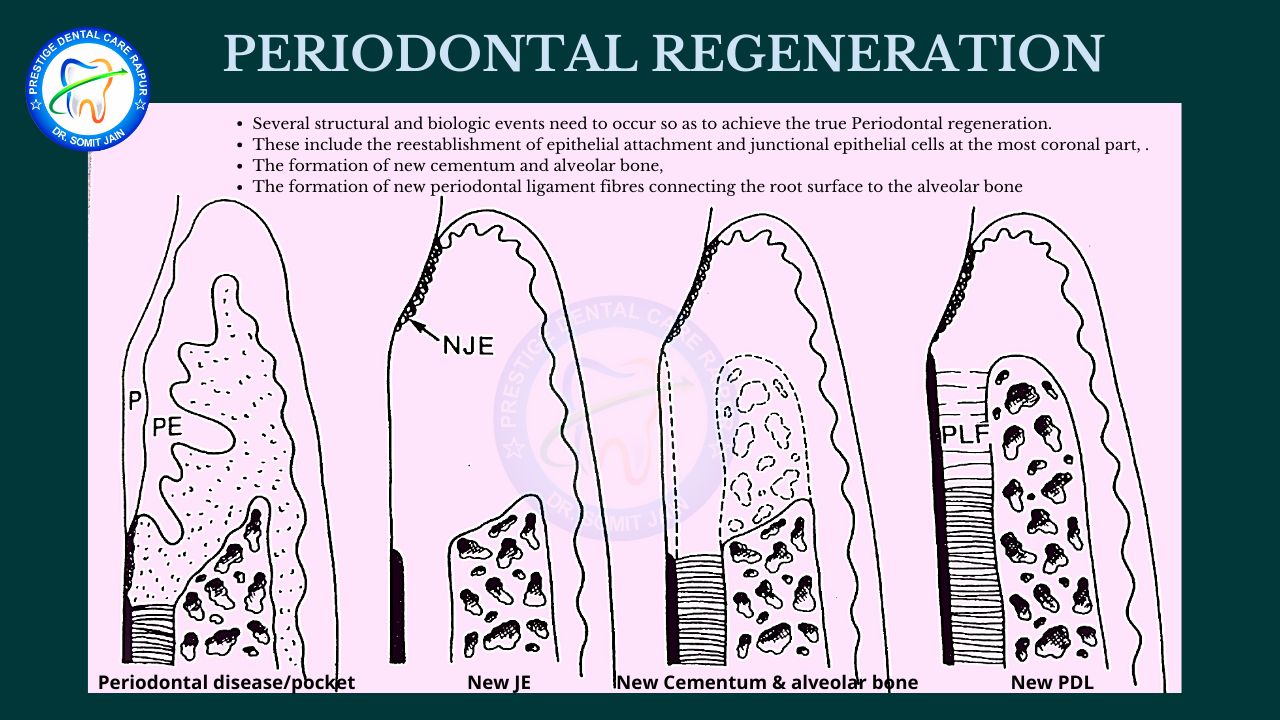
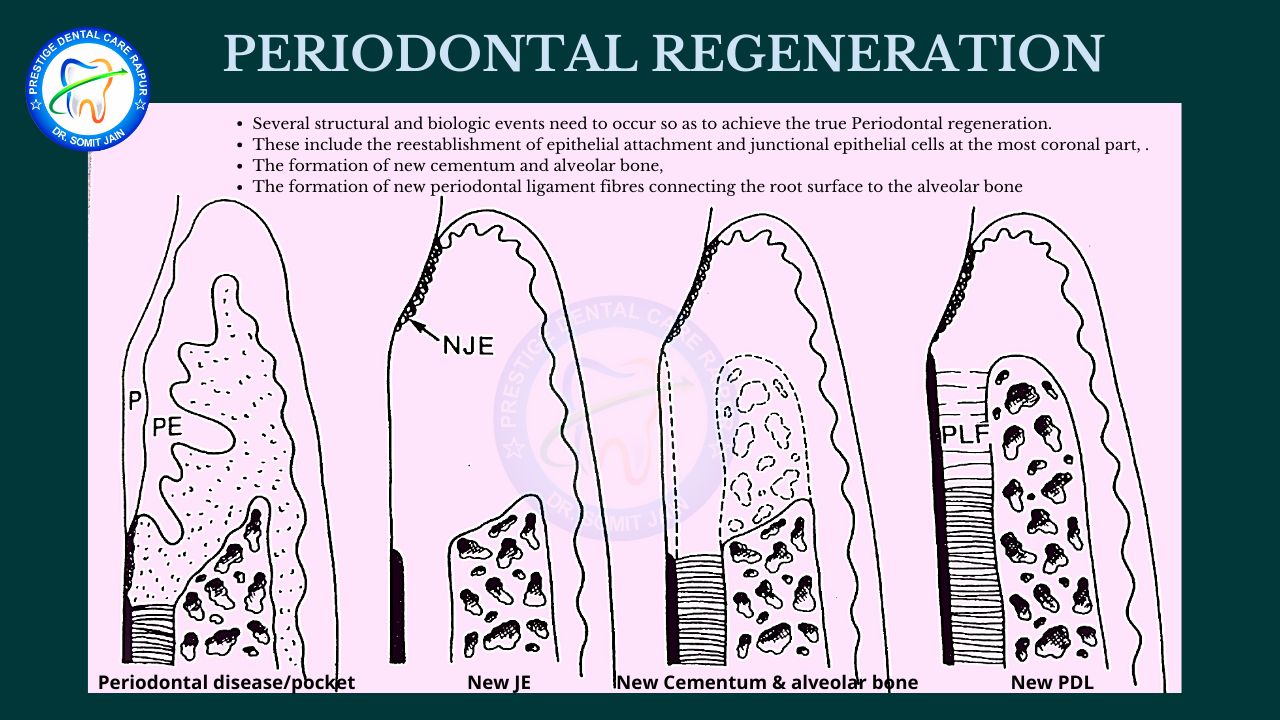
From this concept of compartmentalization, Guided Tissue Regeneration GTR procedures developed and barrier membranes were being utilized to accomplish the goal of epithelial exclusion: cell/tissue re-population control, space maintenance and clot stabilization.
GTR is based on the principle of exclusion of gingival connective tissue cells and the prevention of epithelial downgrowth into the wound.
By exclusion of these gingival tissues, cells with regenerative potential (periodontal ligament, bone cells and possibly cementoblast) can enter the wound site first and promote regeneration.
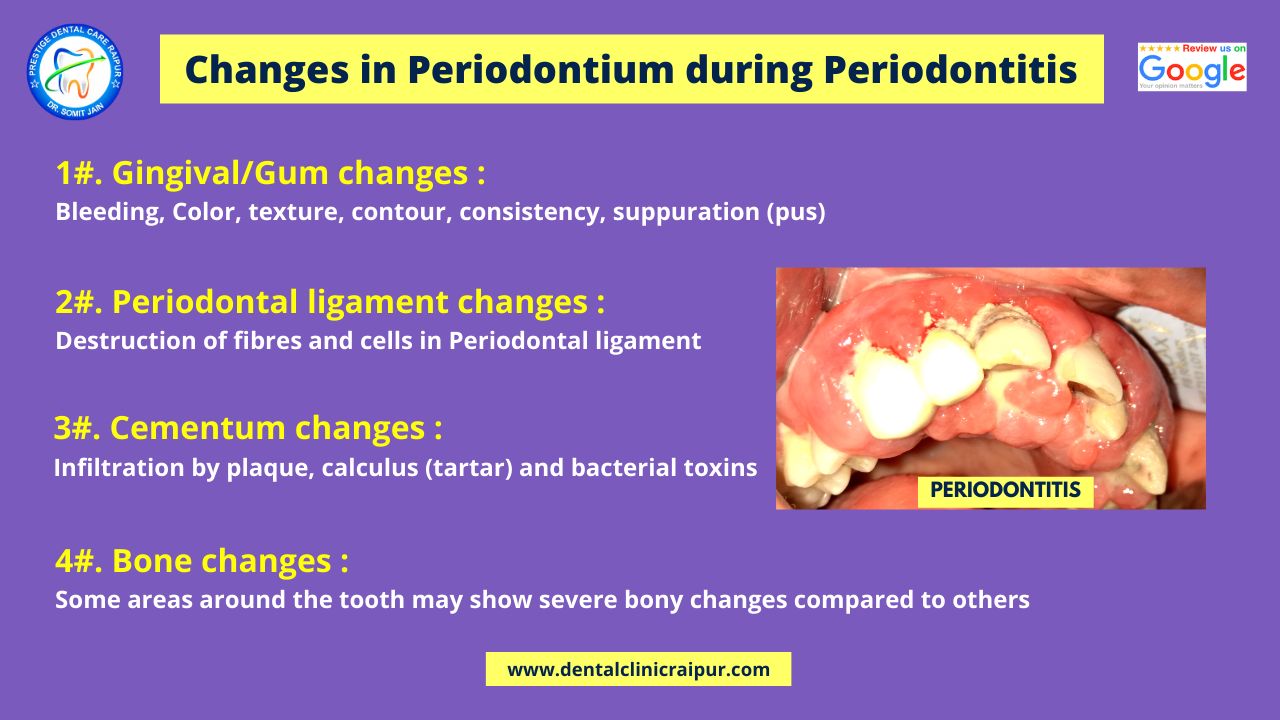
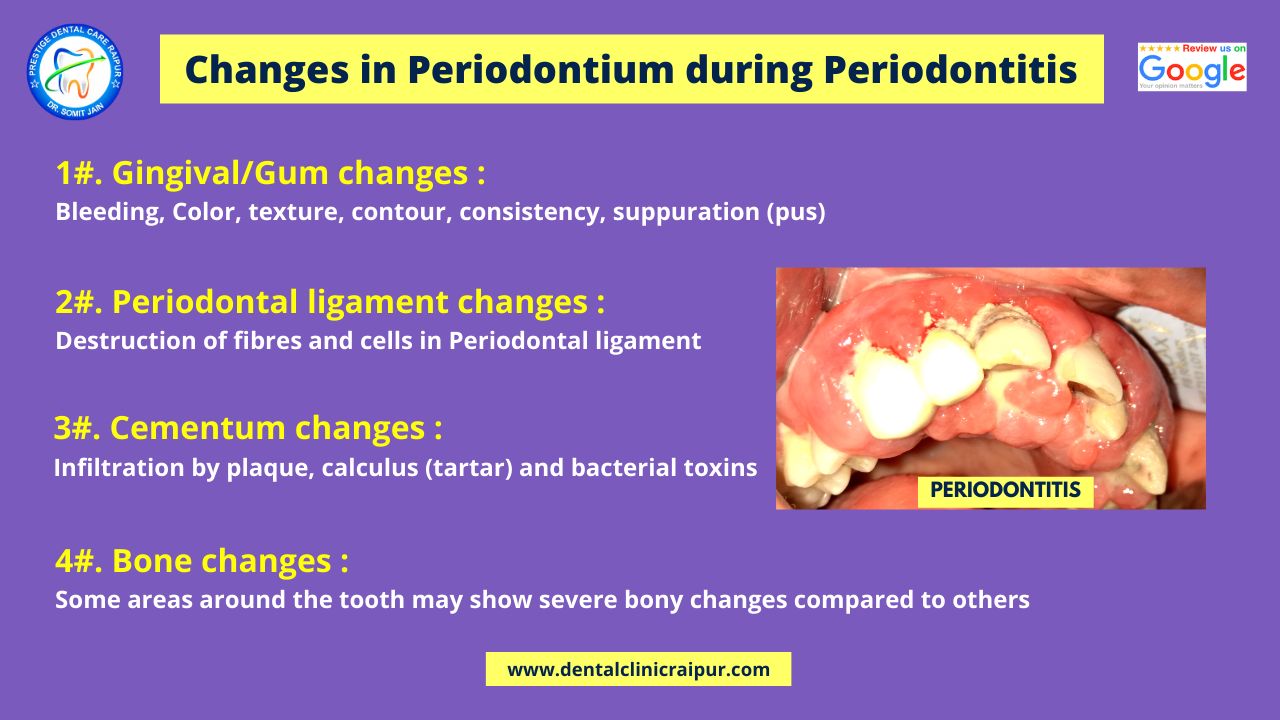
Changes in Periodontium during Periodontitis
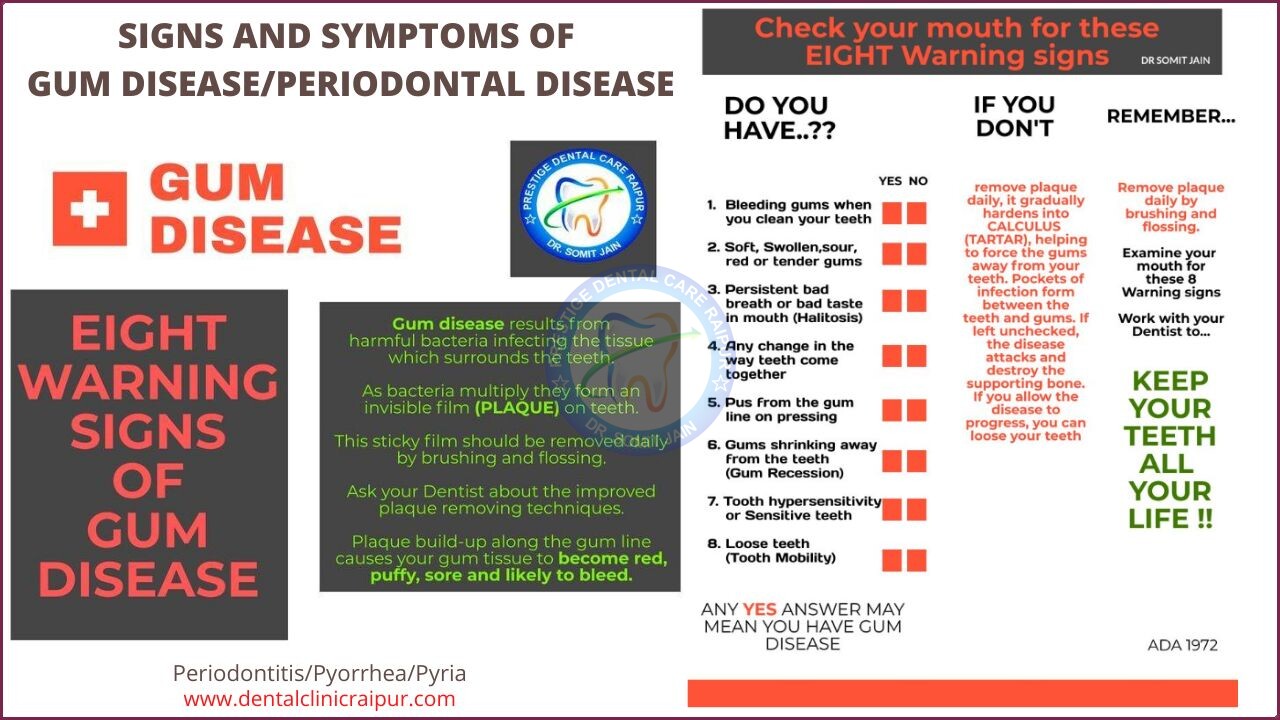
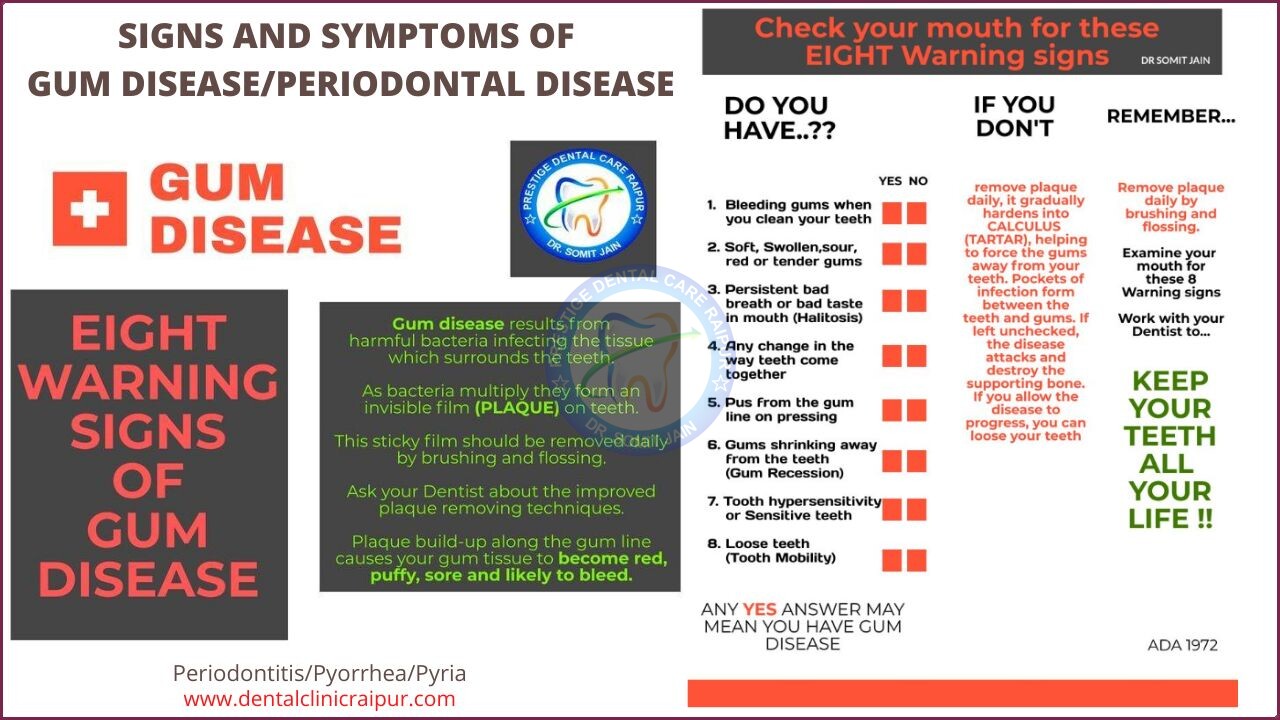
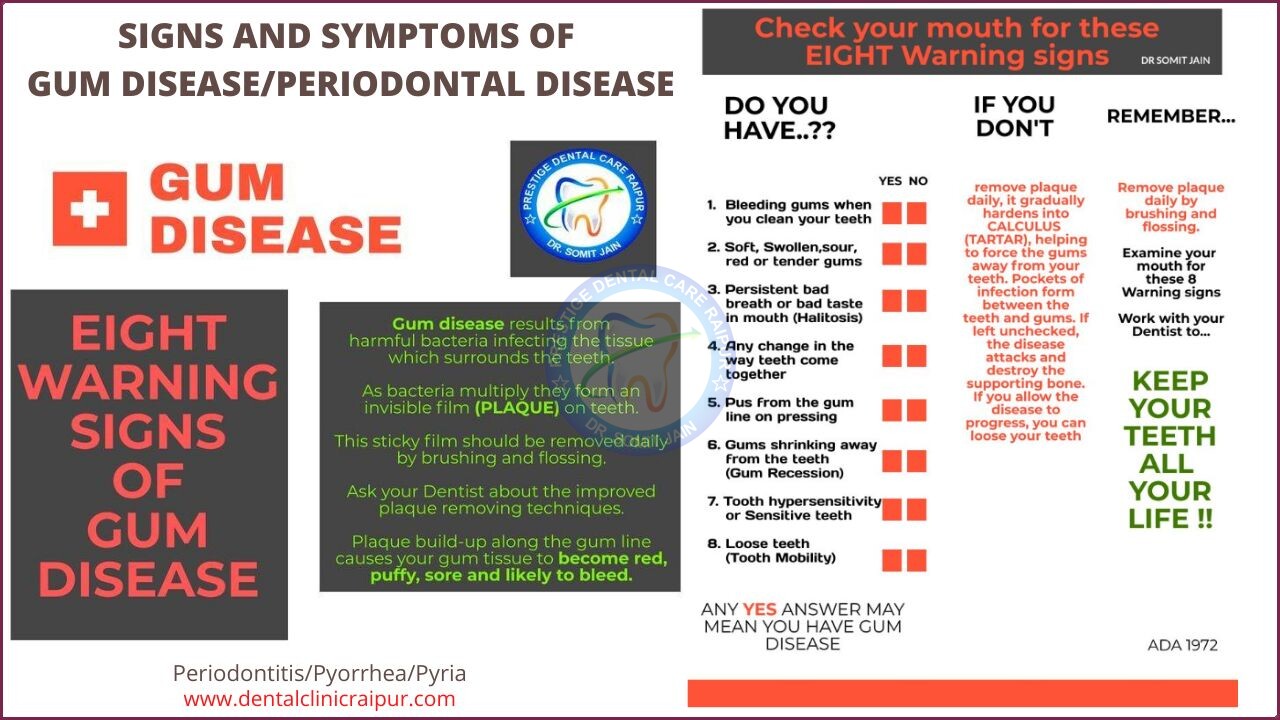
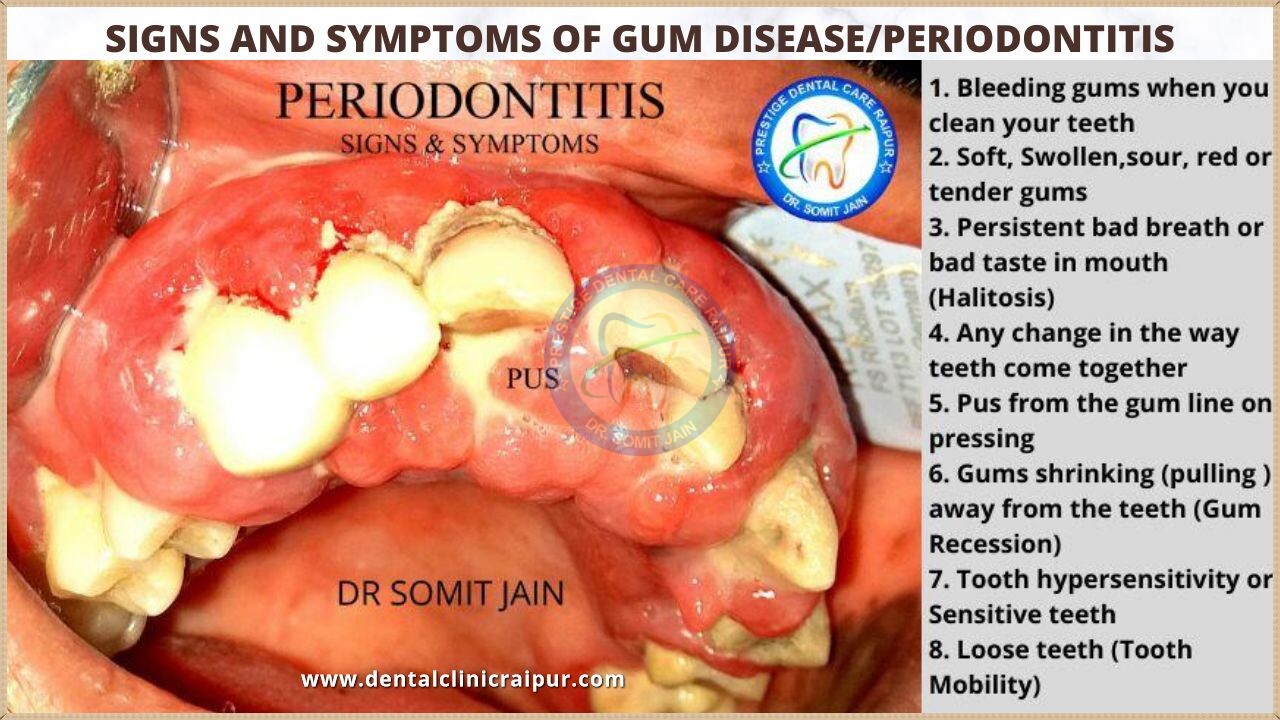
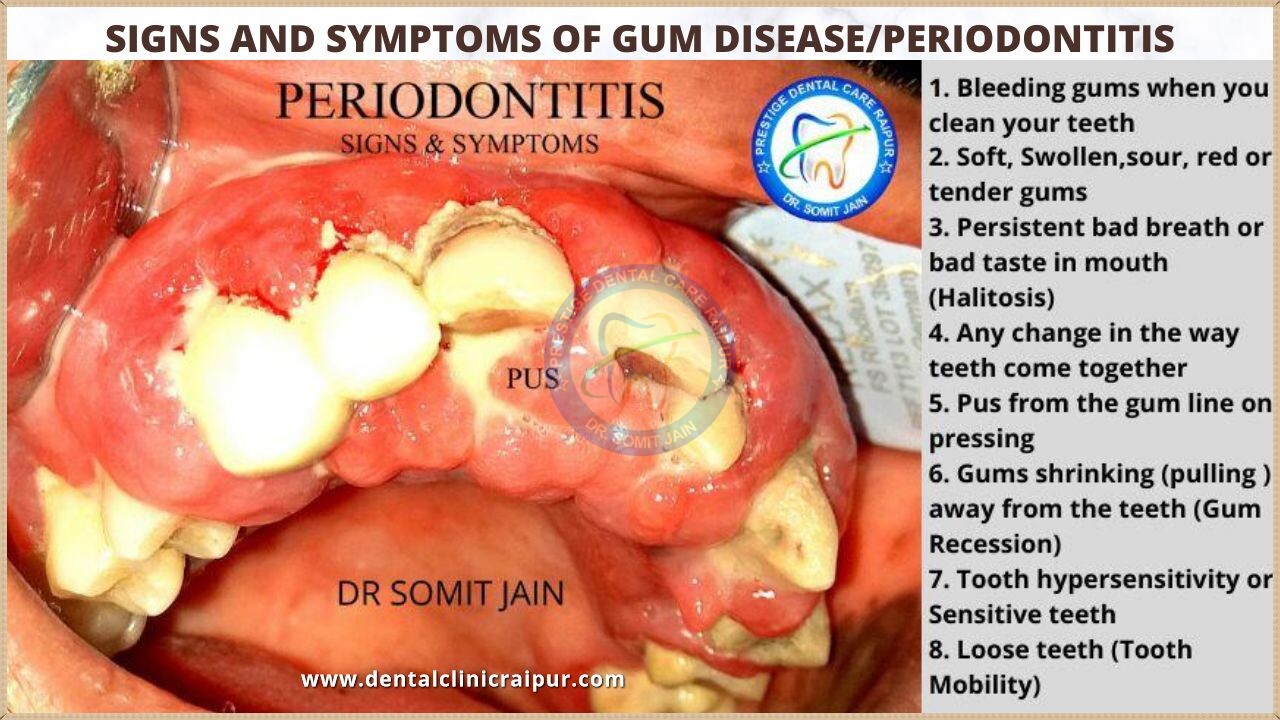
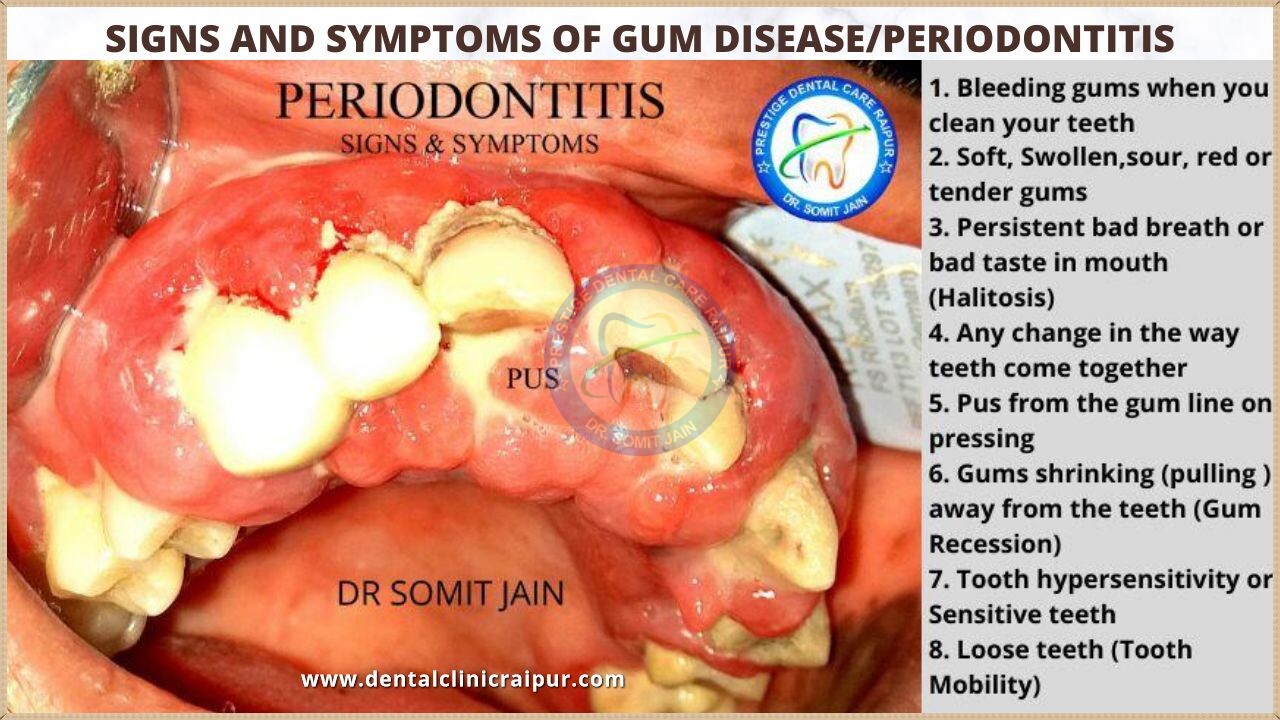
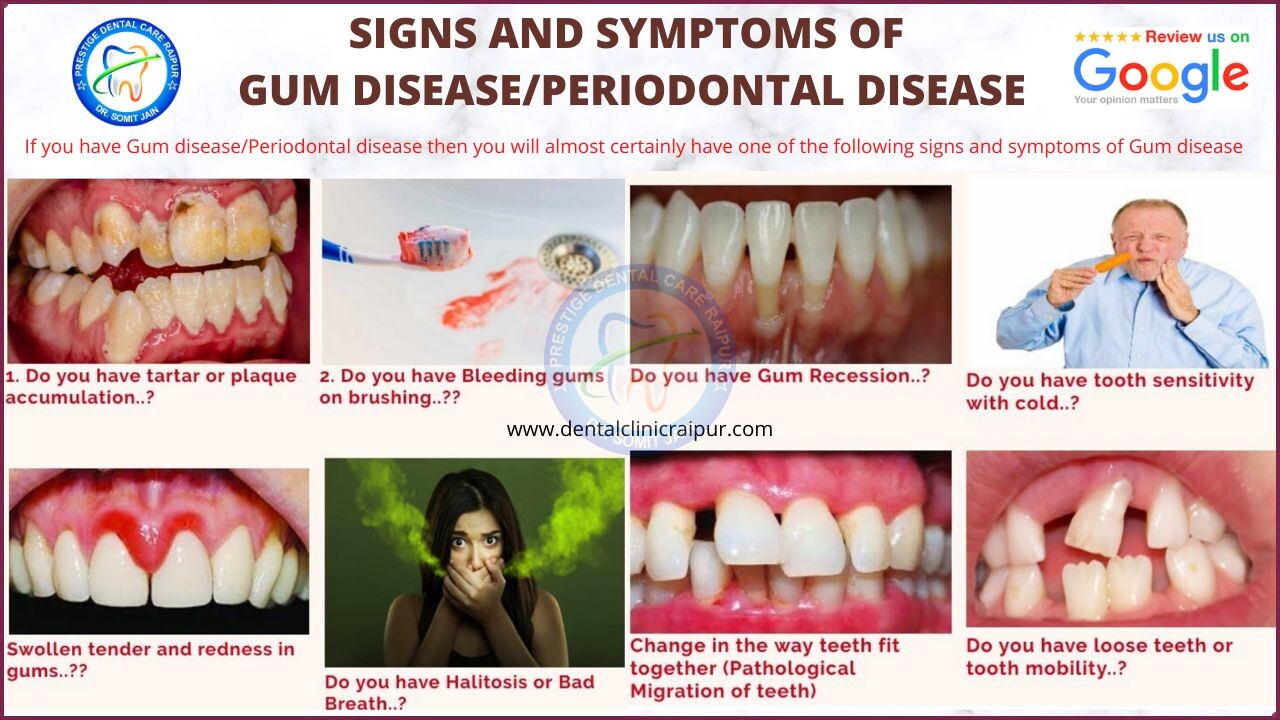
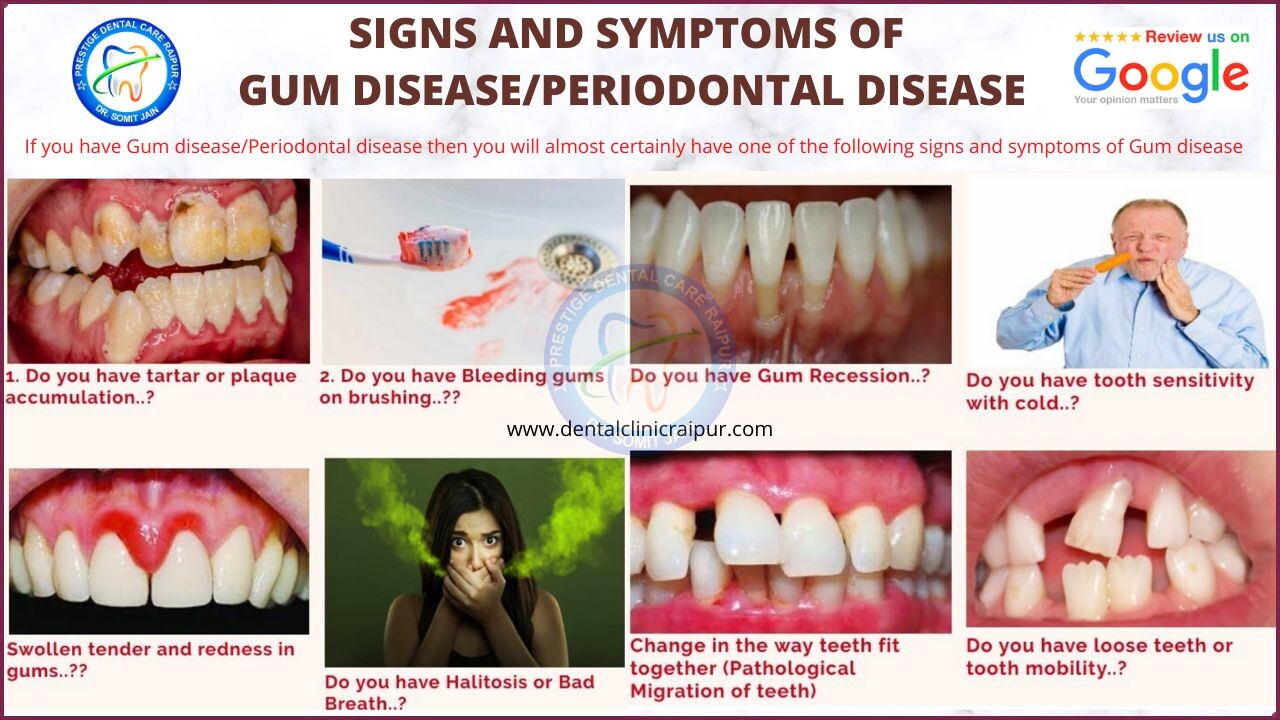
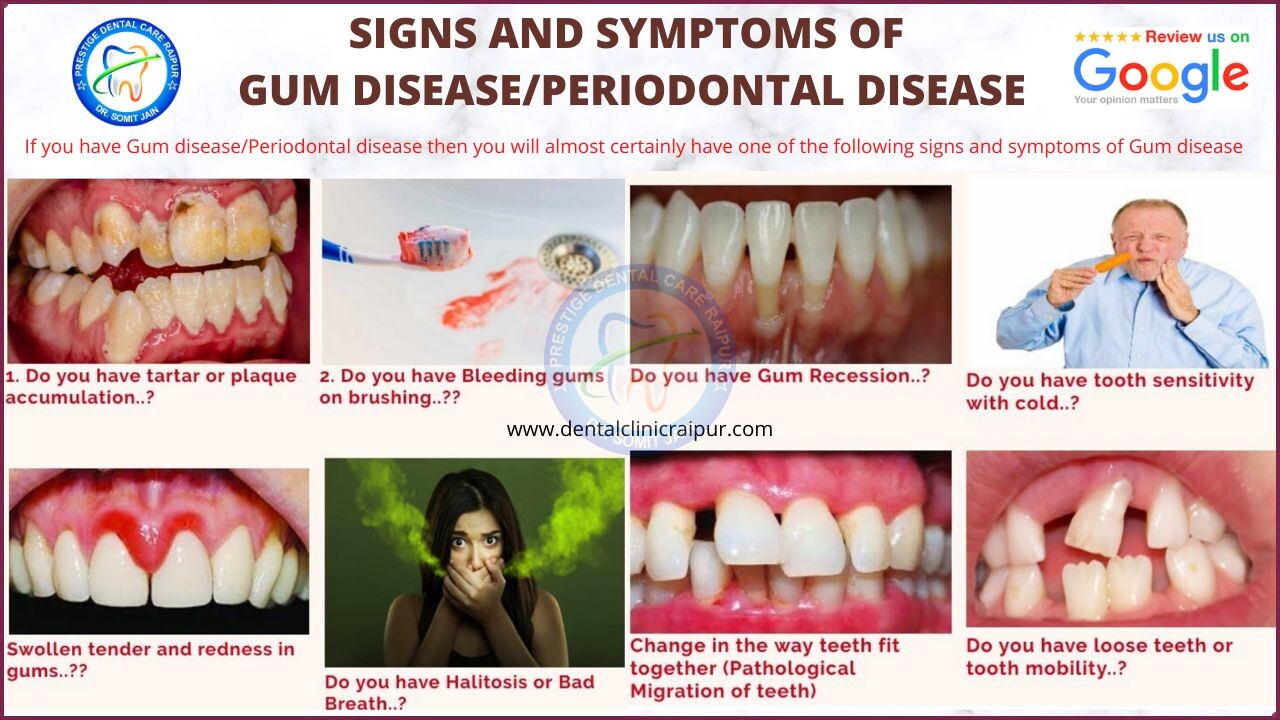
6#. What are the 8 Warning signs and symptoms of Gum Disease/Periodontitis?
Spot the 8 Warning signs of Periodontal disease by Dr.Somit Jain
If you happen to have Gum disease/Periodontal disease then you might very well develop few of below mentioned warning signs and symptoms of Periodontitis including:
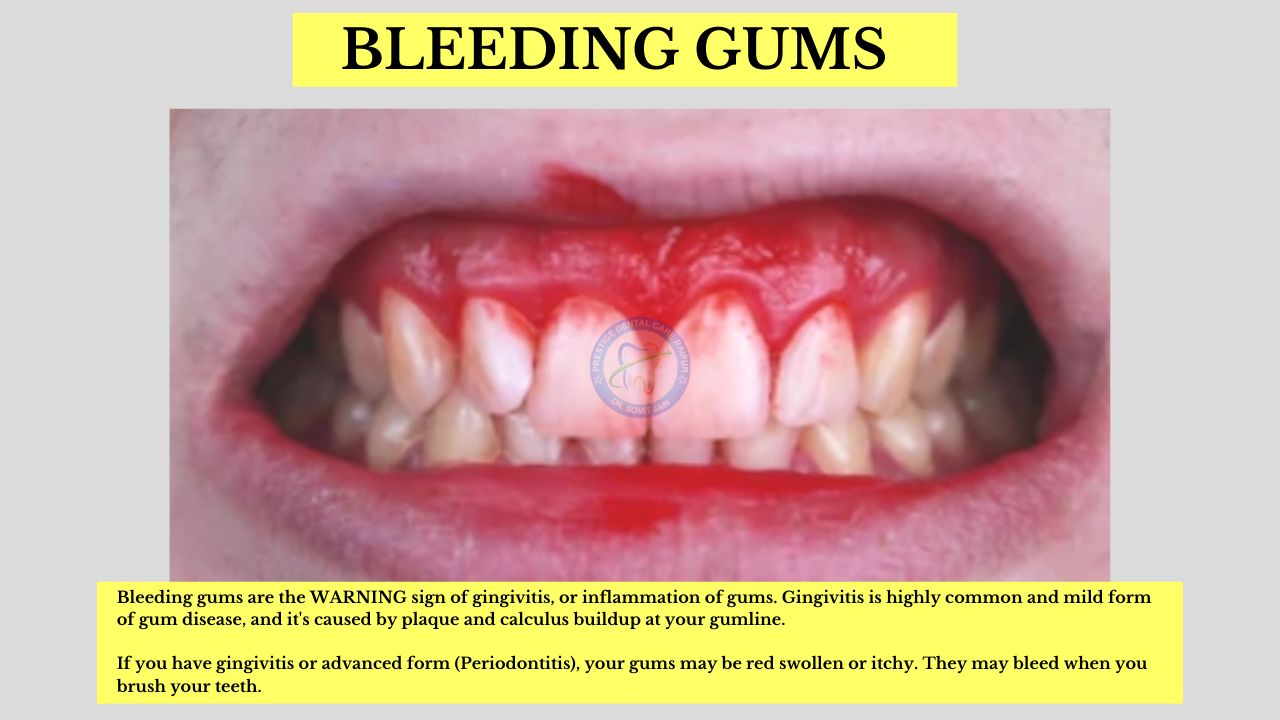
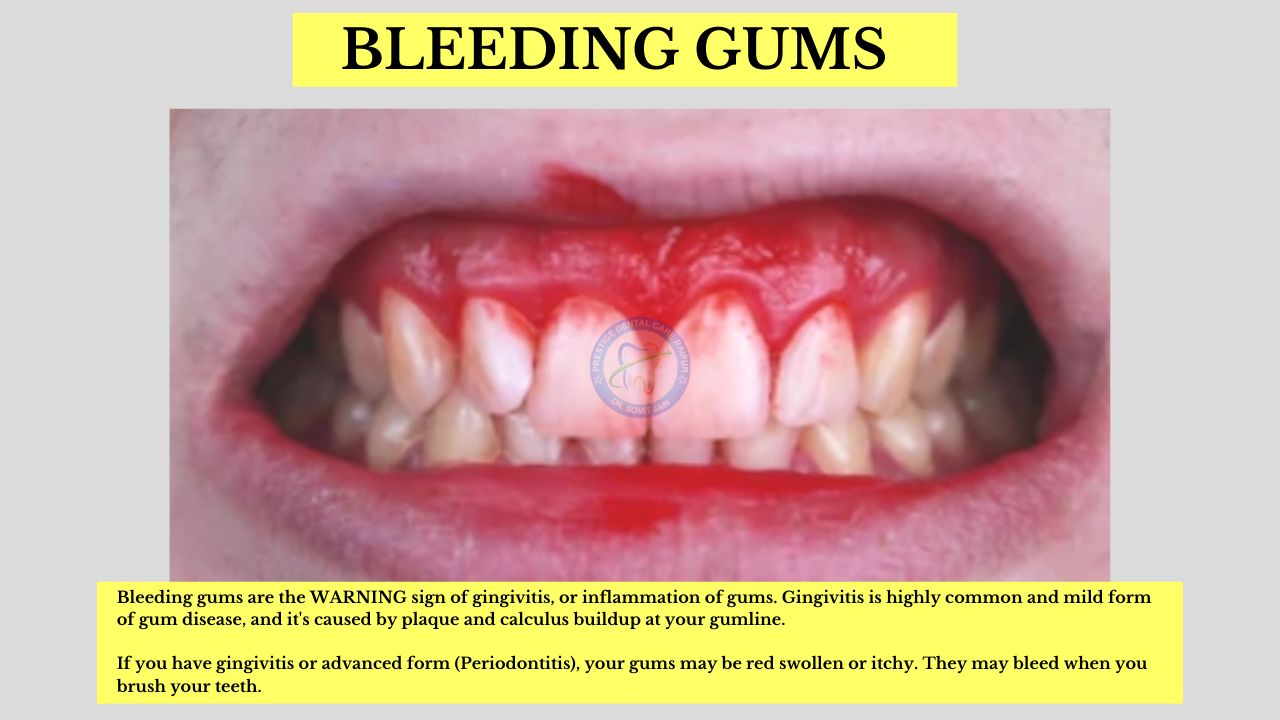
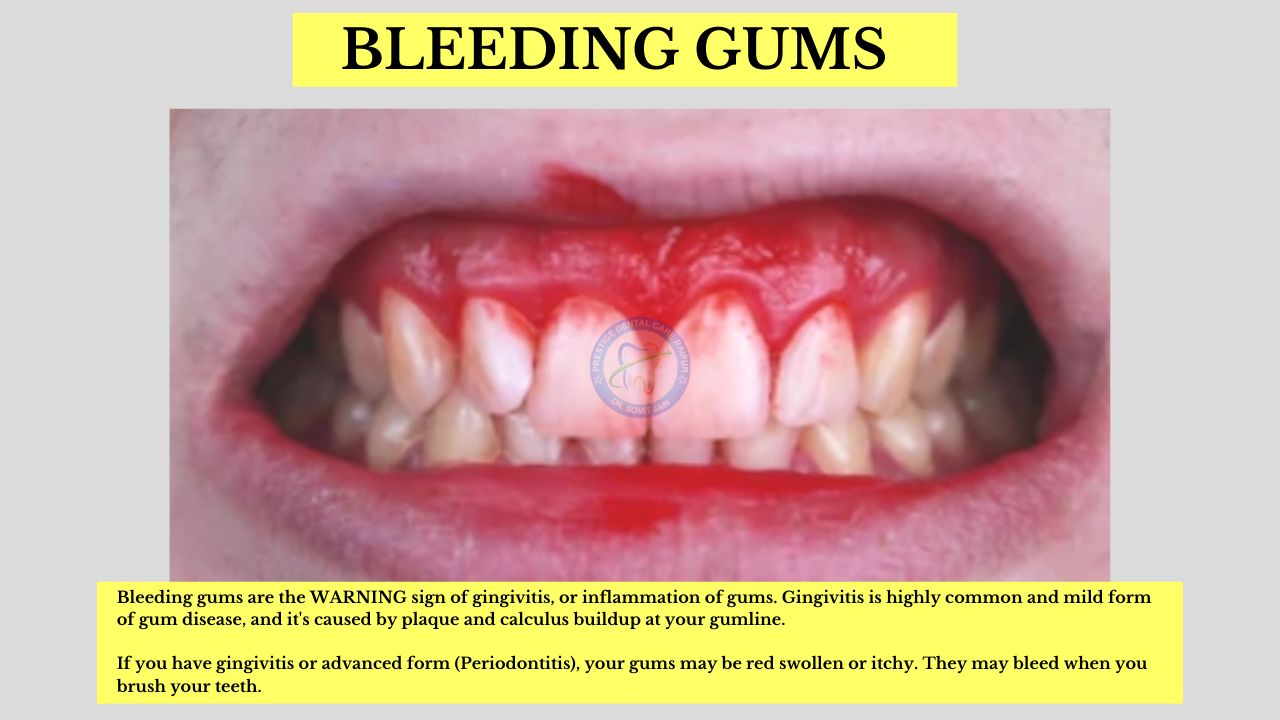
1. Bleeding gums when you clean your teeth (Do you ever spit out “Pink” in the Sink and can u see from where bleeding is coming from?)
2. Gum tissues are rolled out, puffy, soft, Swollen, sour, red or tender
3. Persistent bad breath (Halitosis) or altered taste in mouth
4. Change in your bite (how teeth of both jaws come together)
5. Pus expressed around gum line on slight provocation
6. Pulling away of gums from the teeth (Gum Recession)
7. Tooth hypersensitivity or Sensitive teeth
8. Loose teeth (Tooth Mobility)
Periodontal disease is mostly silent & painless, so with utmost care we need to be aware of above mentioned warning signs.
7#. What are the causes of Gum disease?
- Gum disease can be caused by a number of factors, but poor oral hygiene is the most common cause.
- Poor oral hygiene, such as not brushing your teeth properly or regularly, can cause plaque and calculus to deposit on your teeth.
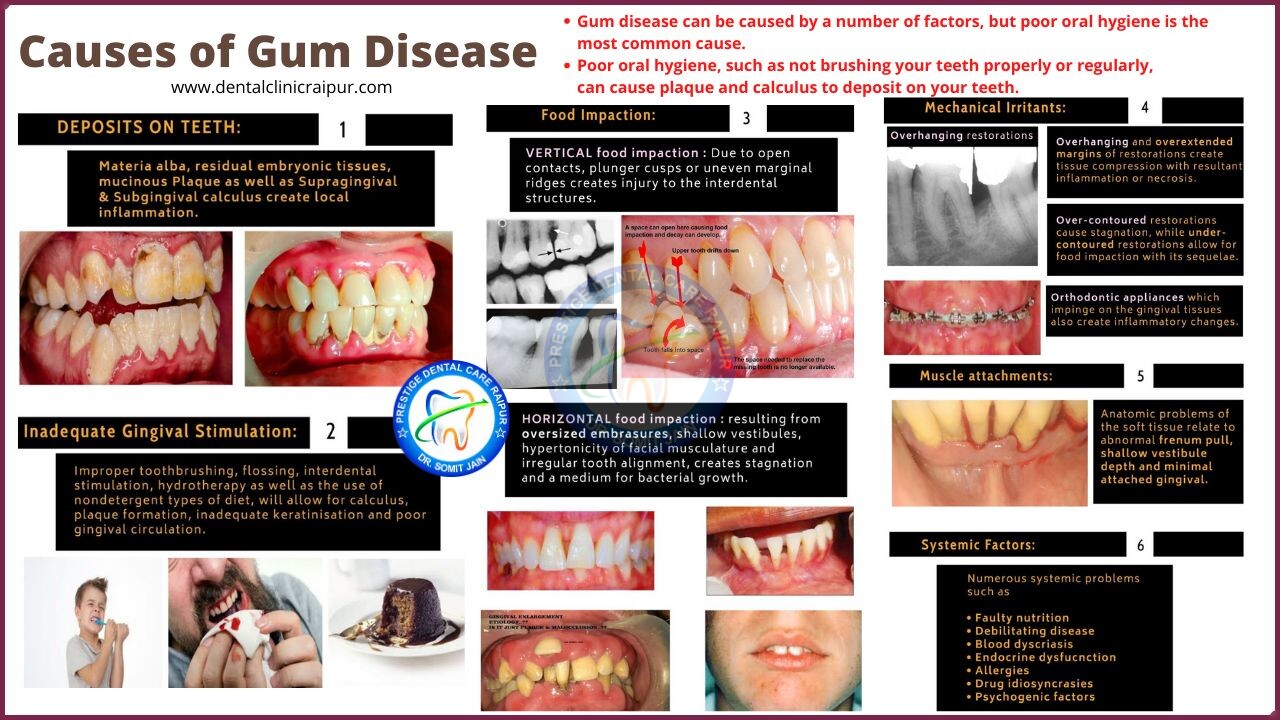
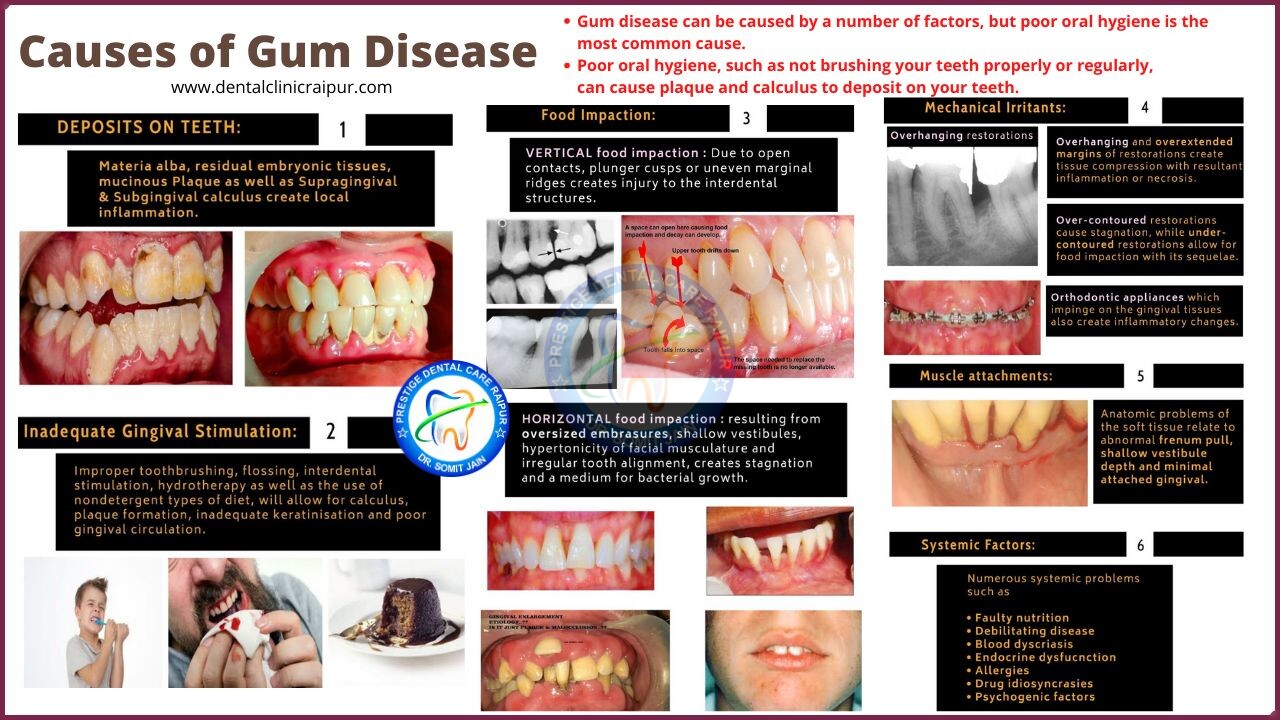
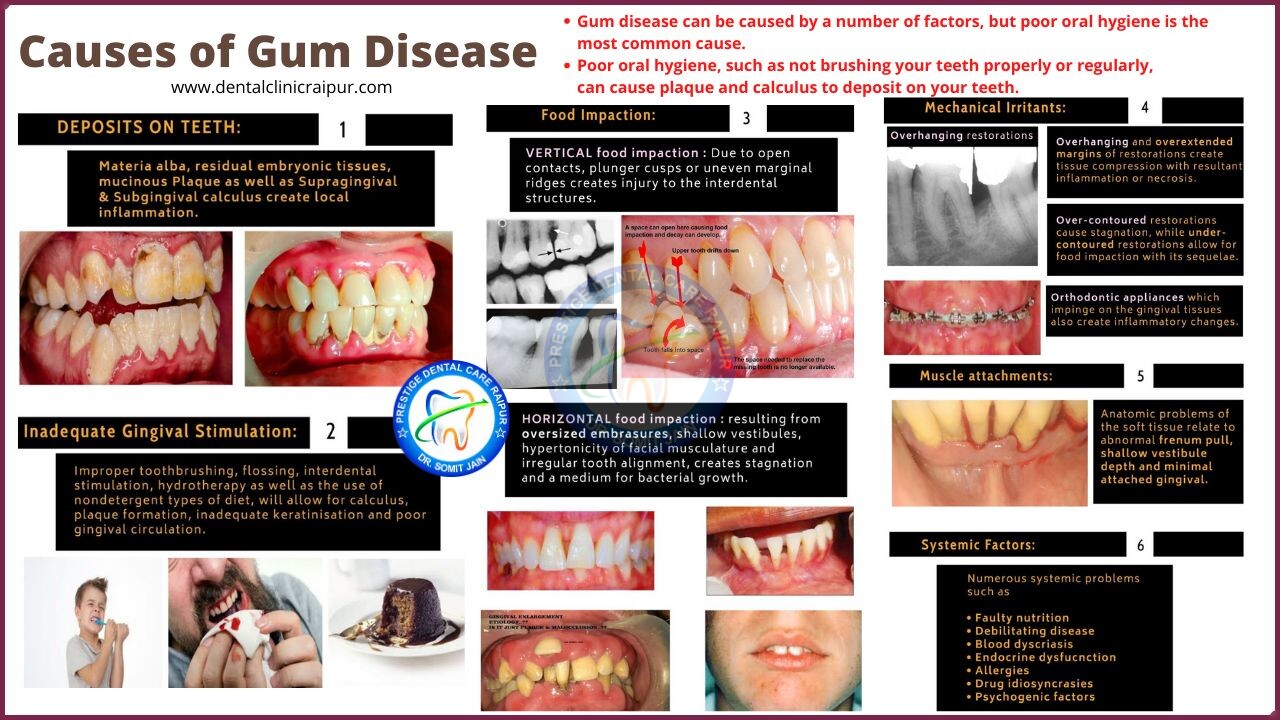
It is generally agreed that all known etiologic factors should be eliminated to effect a maximum response to Periodontal therapy. Among the more common causative agents are:
- DEPOSITS ON TEETH: Materia alba, residual embryonic tissues, mucinous Plaque (biofilm formation with bacteria) as well as Supragingival and Subgingival calculus create local inflammation.
- Inadequate Gingival Stimulation: Improper toothbrushing, flossing, interdental stimulation, hydrotherapy as well as the use of nondetergent types of diet, will allow for calculus, plaque biofilm formation, inadequate keratinisation and poor gingival circulation.
- Food Impaction
- Vertical food impaction : Due to open contacts, plunger cusps or uneven marginal ridges creates injury to the interdental structures.
- Horizontal food impaction : resulting from oversized embrasures, shallow vestibules, hypertonicity of facial musculature and irregular tooth alignment, creates stagnation and a medium for bacterial biofilm growth.
- Overhanging and overextended margins of restorations create tissue compression with resultant inflammation or necrosis.
- Over-contoured restorations cause stagnation, while under-contoured restorations allow for food impaction with its sequelae.
- Orthodontic appliances which impinge on the gingival tissues also create inflammatory changes.
- Overzealous toothbrushing, incorrect in manner or type of brush, may allow for damage to the tooth, gingival and crestal bone.
- Mouth Breathing and Smoking often cause dehydration of the soft tissue with resultant inflammation.
- Faulty nutrition
- Debilitating disease
- Blood dyscriasis
- Endocrine dysfucnction
- Allergies
- Drug idiosyncrasies
- Psychogenic factors
Above plays important role in the etiology of Periodontal disease/Gum disease.
8#. What is the role of Dental Plaque Biofilm in Gum disease/Periodontal disease?
THE ROLE OF DENTAL PLAQUE
- The presence of bacteria in the oral cavity has been known since the time of Anton von Leeuwenhoek, who described the “animalcules” in dental plaque.
- Bacterial etiology of Periodontitis has been explored over 100 years evolving along with technologies advances in identification and characterization.
- One of the most significant recent developments in the understanding of periodontal disease etiology is the recognition of dental plaque as a BIOFILM.
- A biofilm is defined as single cells and micro-colonies enclosed in a highly hydrated, predominantly anionic exopolymer matrix. These sessile cells behave in profoundly different ways from the free floating (planktonic) counterparts.



DENTAL PLAQUE AS A BIOFILM-DEVELOPMENT
- Plaque formation follows several distinct phases, beginning with adsorption onto the tooth surface of a conditioning film derived from bacterial and host molecules that forms immediately following tooth eruption or tooth cleaning.
- This adsorption is followed by passive transport of bacteria mediated by weak, long-range forces of attraction.
- The primary colonizers form a biofilm by autoaggregation (attraction between same species) and coaggregation (attraction between different species)
- Coaggregation results in a functional organization of plaque bacteria and formation of different morphologic structures such as corncobs and rosettes. The microenvironment now changes from aerobic/capnophilic to facultative anaerobic.
- The attached bacteria multiply and secrete an extracellular matrix which results in a mature mixed-population biofilm.
SOME OF THE PROPERTIES OF A BIOFILM
- CELL-CELL COMMUNICATION
- GENE TRANSFER
- ANTIMICROBIAL RESISTANCE
- REGULATION OF GENE EXPRESSION
- BACTERIAL ANTIGENS & VIRULENCE FACTORS
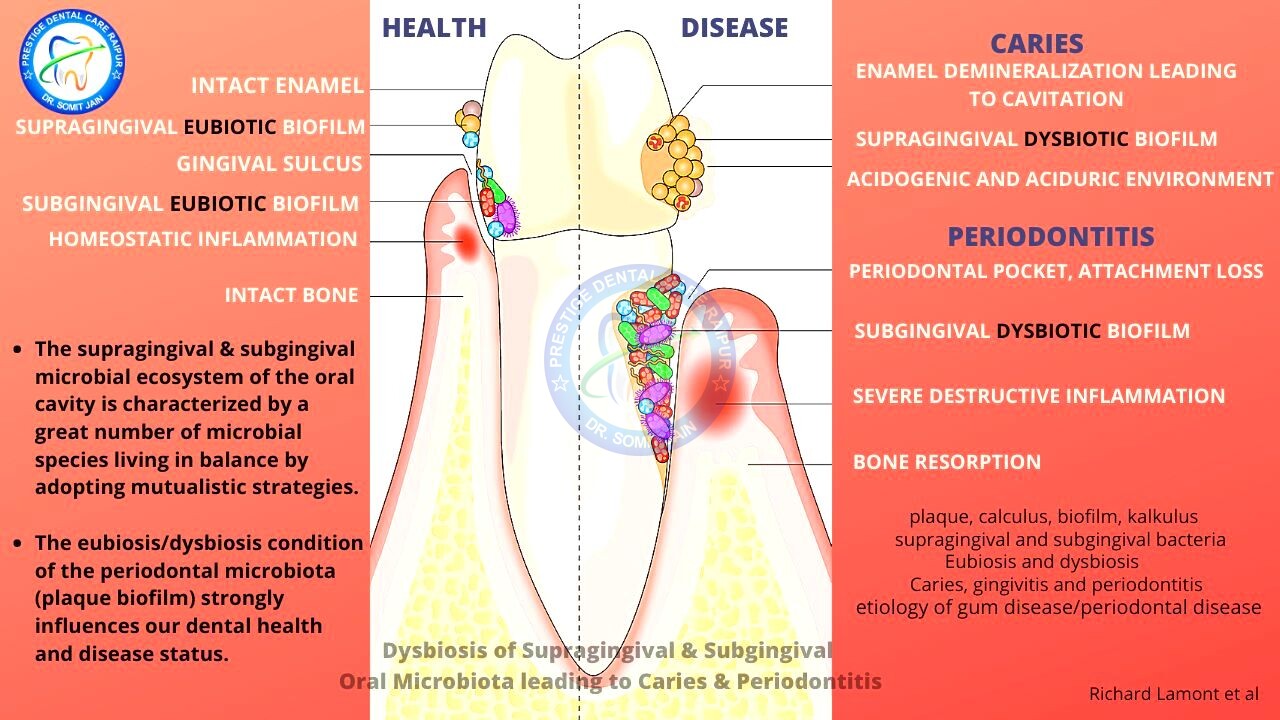
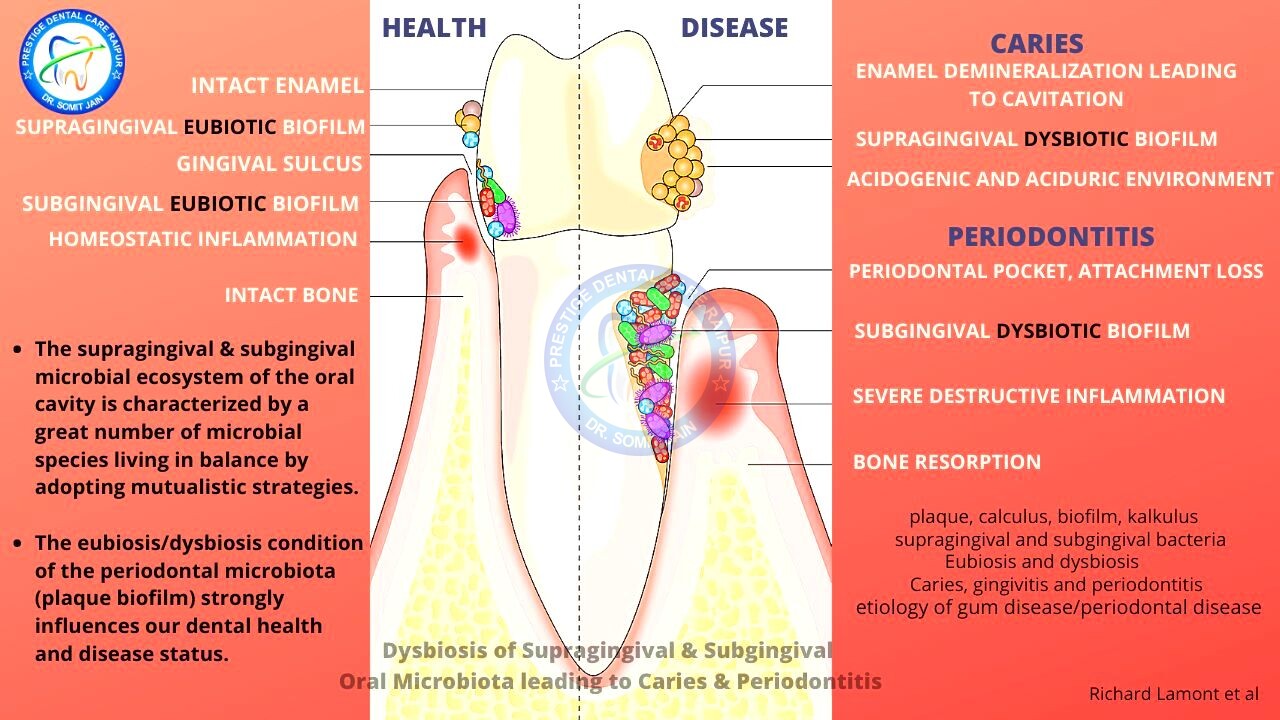
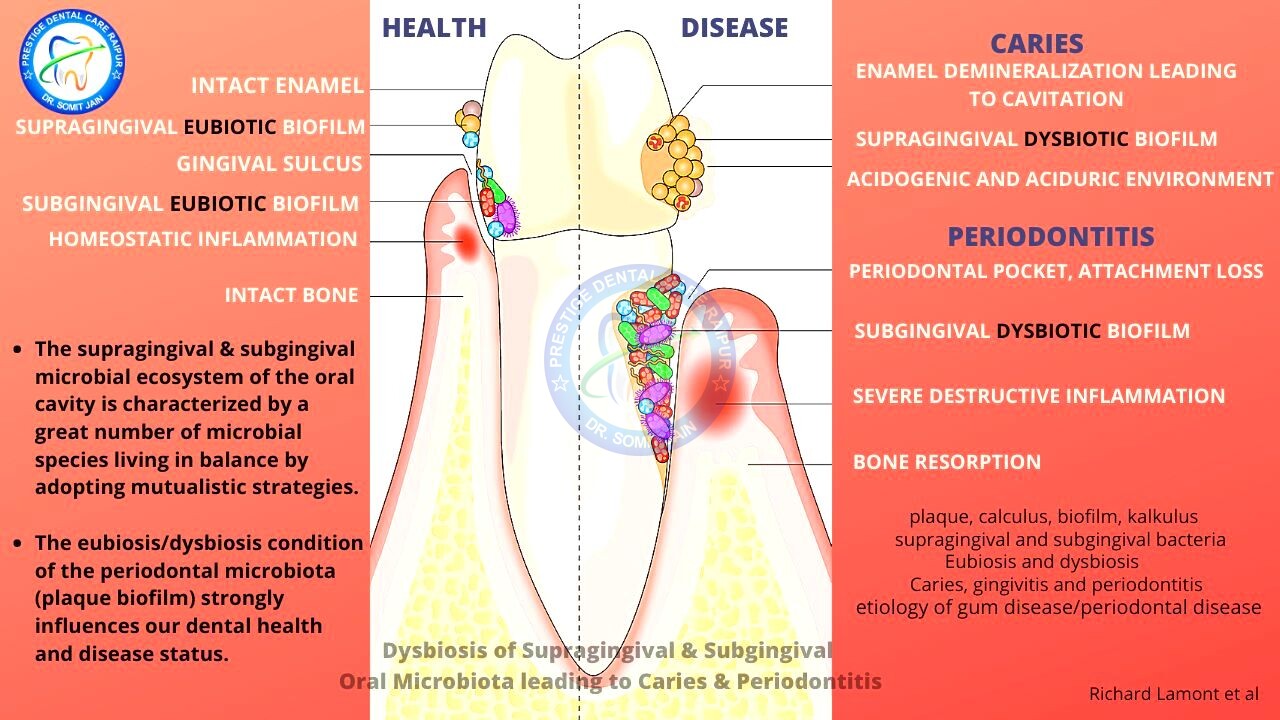
8#. Dysbiosis of Supragingival & Subgingival Oral Microbiota leading to Caries & Periodontitis
- The supragingival & subgingival microbial ecosystem of the oral cavity is characterized by a great number of microbial species living in balance by adopting mutualistic strategies.
- The eubiosis/dysbiosis condition of the periodontal microbiota (plaque biofilm) strongly influences our dental health and disease status.
Periodontal bacteria in health and disease
- Gingivitis is a plaque induced inflammatory process of gingival epithelium and connective tissue surrounding the teeth with no loss of attachment.
- The inflammatory process in Gingivitis does not extend into supporting Periodontium i.e. the cementum, periodontal ligament and bundle bone.
- The primary etiologic agent of Gingivitis is Dental plaque biofilm and considered to be the most benign form of gum disease.
- The secondary etiologic factor for Gingivitis may include stress, anxiety, lowered resistance, nutritional impairment, mouth breathing, smoking and gross neglect.
- Plaque associated Gingivitis may have one or more of the following clinical signs and symptoms including bleeding upon probing or spontaneous, bad breathe or halitosis, gingival sensitivity and itching.
- Gingivitis by definition has no loss of attachment or radiographic loss of bone.
- According to Page and Schroeder (1976) concept of the pathogenesis of the periodontal lesion, the first three stages (initial, early & established lesion) are consistent with the clinical diagnosis of gingivitis.
- Periodontitis can be defined as inflammation involving the muco-gingival unit (gingiva and alveolar mucosa) and may extend to the supporting periodontium including the cementum periodontal ligament and alveolar bone proper.
- Periodontitis/Gum disease is initiated by DYSBIOSIS (imbalance) of the complex dental plaque biofilm on the supra and subgingival surfaces of teeth and gingiva.
- The plaque-induced variety of Gum disease (Gingivitis & Periodontitis) are extremely prevalent chronic immuno-inflammatory conditions that may affect various components of the Periodontium including gums and bone.
- Gingivitis is more benign of the two conditions where the inflammatory process is limited to the gingival epithelium and connective tissue.
- In contrast, the hallmark of Periodontitis is an immunoinflammatory infiltrate of the deeper compartments of the periodontium, resulting in destruction of the tooth-supporting tissues (Lamina propria of gingiva, cementum, periodontal ligament and alveolar bone), tooth mobility and, ultimately, tooth loss.
- Gingivitis precedes Periodontitis, but it is clear that NOT all cases of Gingivitis progress to advanced form of periodontal disease.
Periodontal disease results from a complex interplay between the subgingival biofilm and the host immune-inflammatory events in response to the challenge presented by the bacteria.
Periodontitis begins with the inflammation and irritation of the gingival tissues which surround and support the teeth. The cause of this inflammation is the toxins released by harmful bacteria found in accumulations of tooth associated materials (plaque biofilm and calculus)
- Periodontitis is a complex multifactorial immuno-inflammatory disease associated with bacteria-host immune system–mediated dysbiosis and characterised by progressive destruction of tooth supporting structure.
- Primary features of Periodontitis include the loss of periodontal tissue support manifested through clinical attachment loss and radiographic bone loss, the presence of periodontal pocketing and gingival bleeding.
- If treated promptly, the effects of mild inflammation (known as gingivitis) are completely reversible.
- However, if the bacterial infection is allowed to progress (poor dental hygiene) or left untreated, Gingivitis may proceed to or risk of developing Periodontitis (Mild, Moderate & Severe) causing the destruction of gum tissue and the underlying jaw bone; promoting tooth loss. Hence Professional Cleaning both above and below the gum line at early stage of disease is very necessary to prevent tooth loss.
- In some cases, the bacteria from this infection can travel to other areas of the body via the bloodstream causing Systemic diseases.
- In most cases, people experience NO PAIN with Periodontitis in early stages until the disease is very advanced. (Periodontal Disease: Don’t Wait Until it Hurts)
- Bleeding and swollen gums are the most common signs & symptoms of developing Periodontitis.
- Risk factors include Smoking, Diabetes, family history, and certain medications.
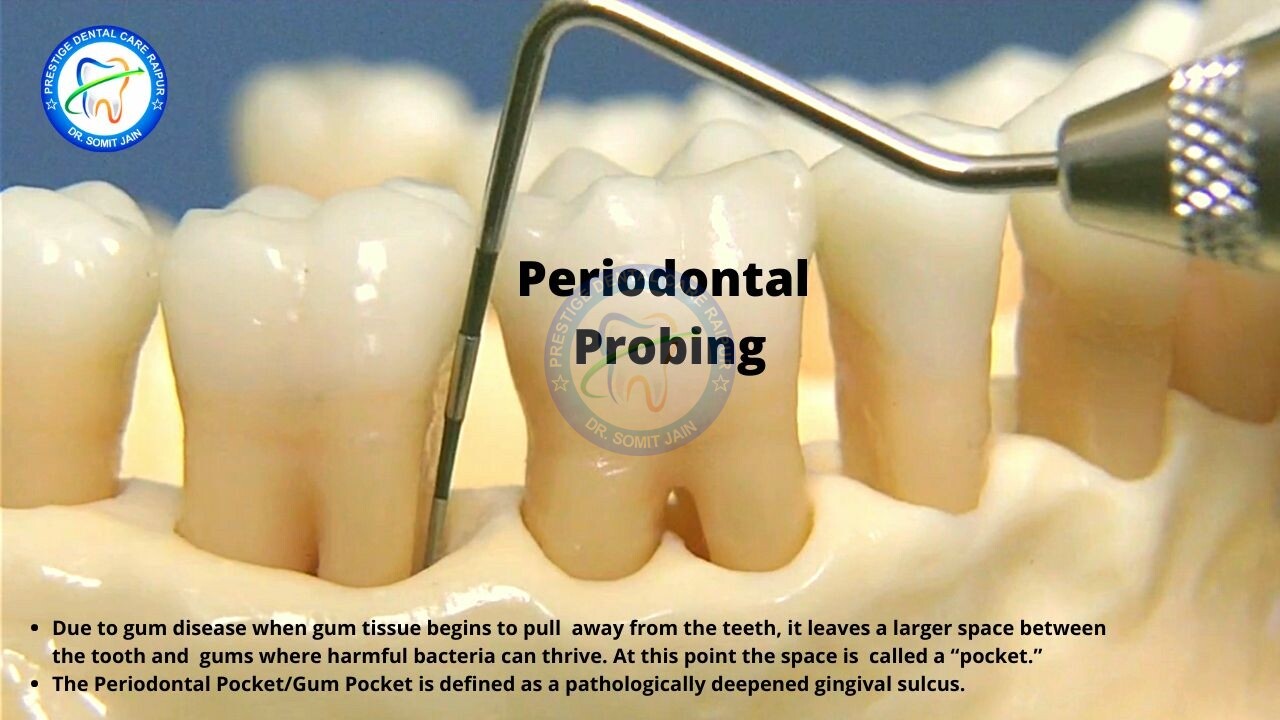
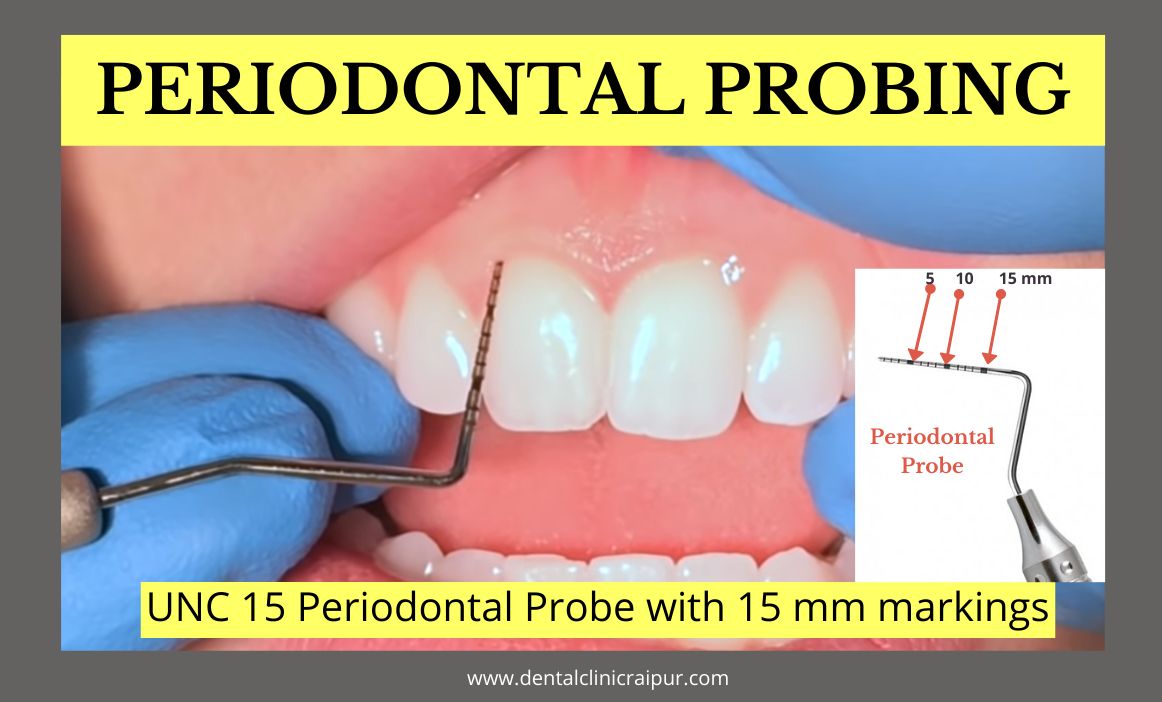
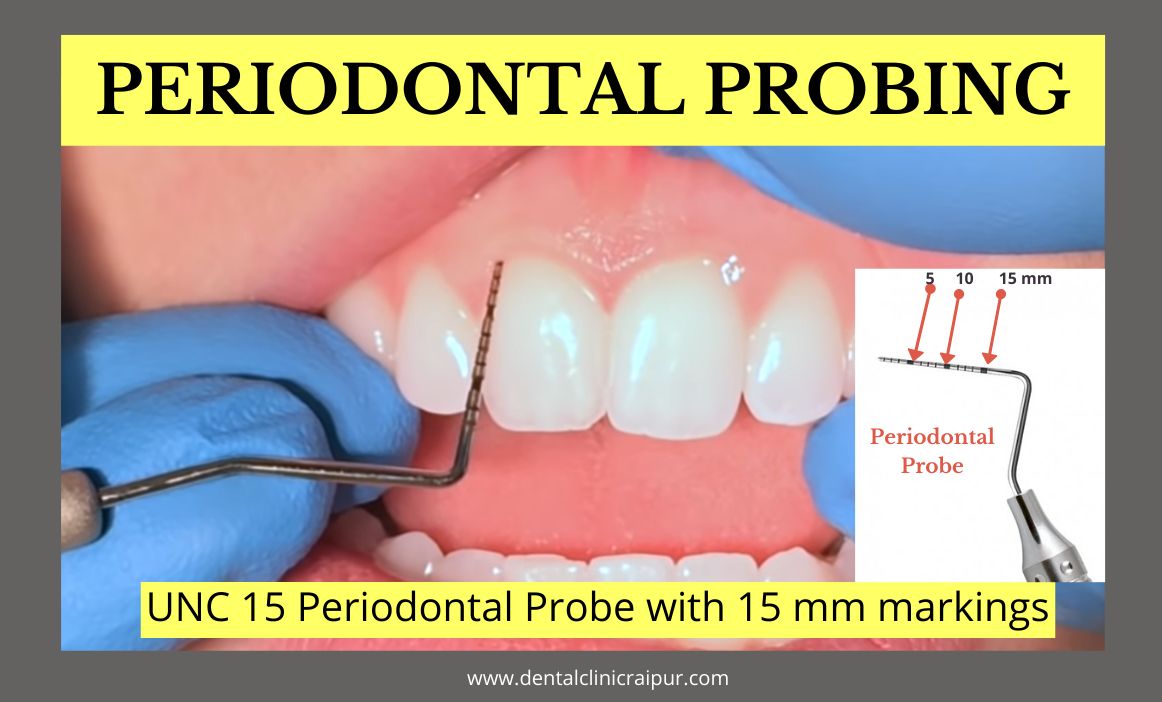
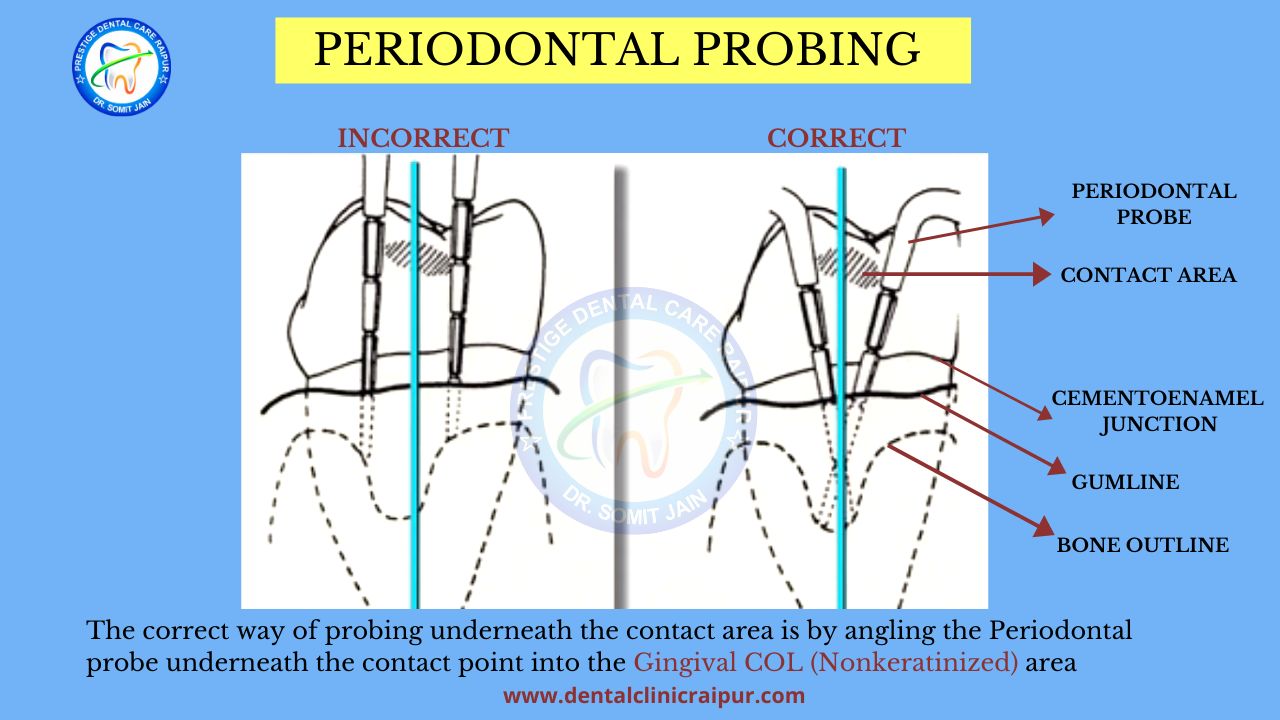
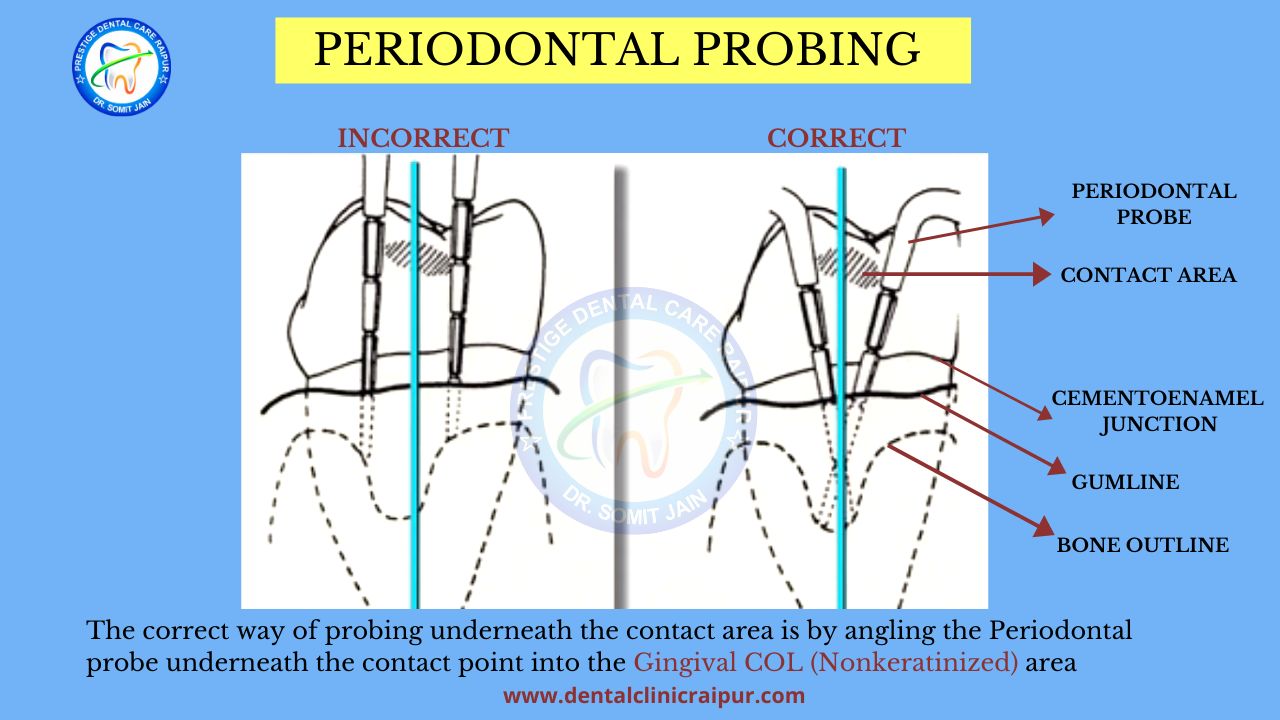
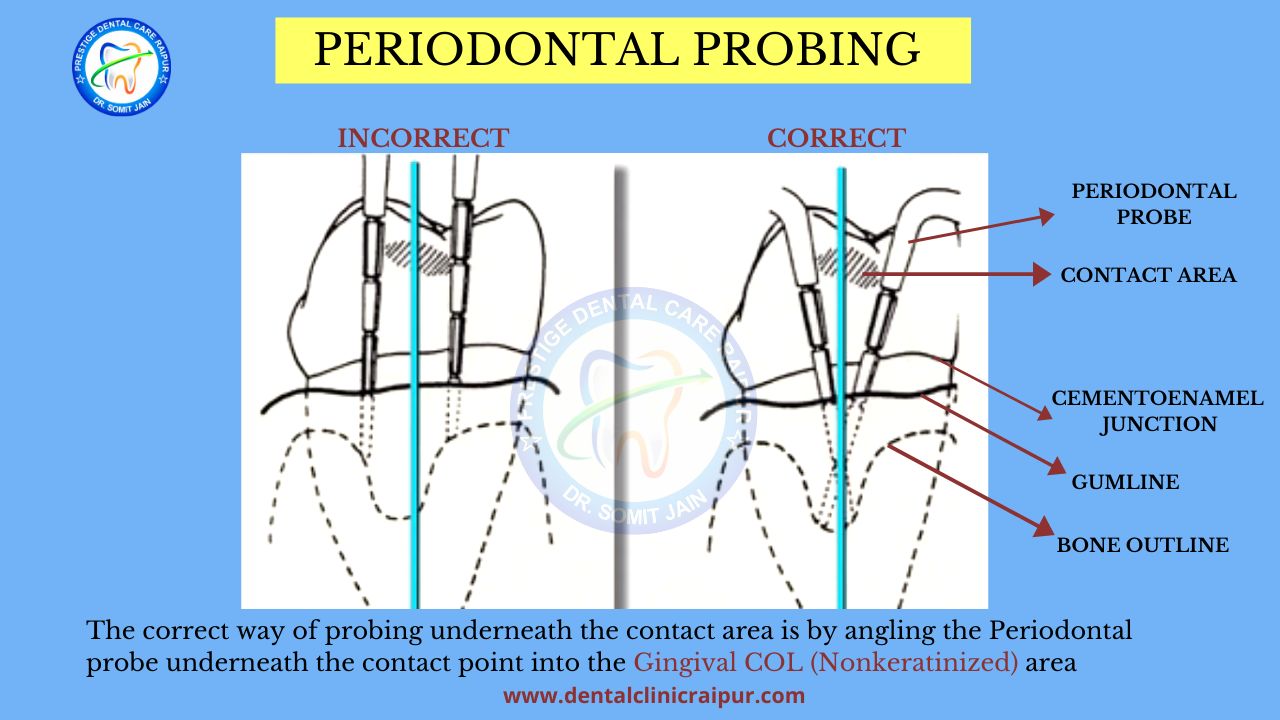
- Diagnosis is made by clinical examination of the gum tissue around the teeth both visually and with a Periodontal Probe (to rule out pockets) and X-rays (IOPA & OPG) looking for bone loss around the teeth.
- If you notice that your gums bleed on a regular basis contact Periodontist or Gum Specialist as soon as possible.
- Regular dental check-ups and proactive preventive good oral hygiene are the best methods for preventing Periodontitis.
- Gingivitis and Periodontitis are inflammatory condition of infectious nature.
- The unequivocal role of bacterial Dental Plaque in the development of these diseases was established 50 years ago.
- Gingivitis is a REVERSIBLE inflammatory reaction of the marginal gingiva to plaque accumulation whereas Periodontitis is a destructive, NON-REVERSIBLE condition resulting in the loss of tooth connective-tissue attachment to bone, which ultimately leads to loss of the involved teeth.
- Existing evidence indicates that Gingivitis precedes the onset of Periodontitis; however not all Gingivitis can develop into Periodontitis. The reason for this is that accumulation of plaque bacteria is necessary but not sufficient by itself for the development of Periodontitis: a susceptible host is necessary. (Tatakis et al)
PRIMARY CLINICAL FEATURE OF PERIODONTITIS
DENTAL PLAQUE-TARTAR-CALCULUS
The biofilms on the supra and subgingival surfaces of the teeth are composed of complex microbial communities which have evolved to inhabit these specialized oral environments.
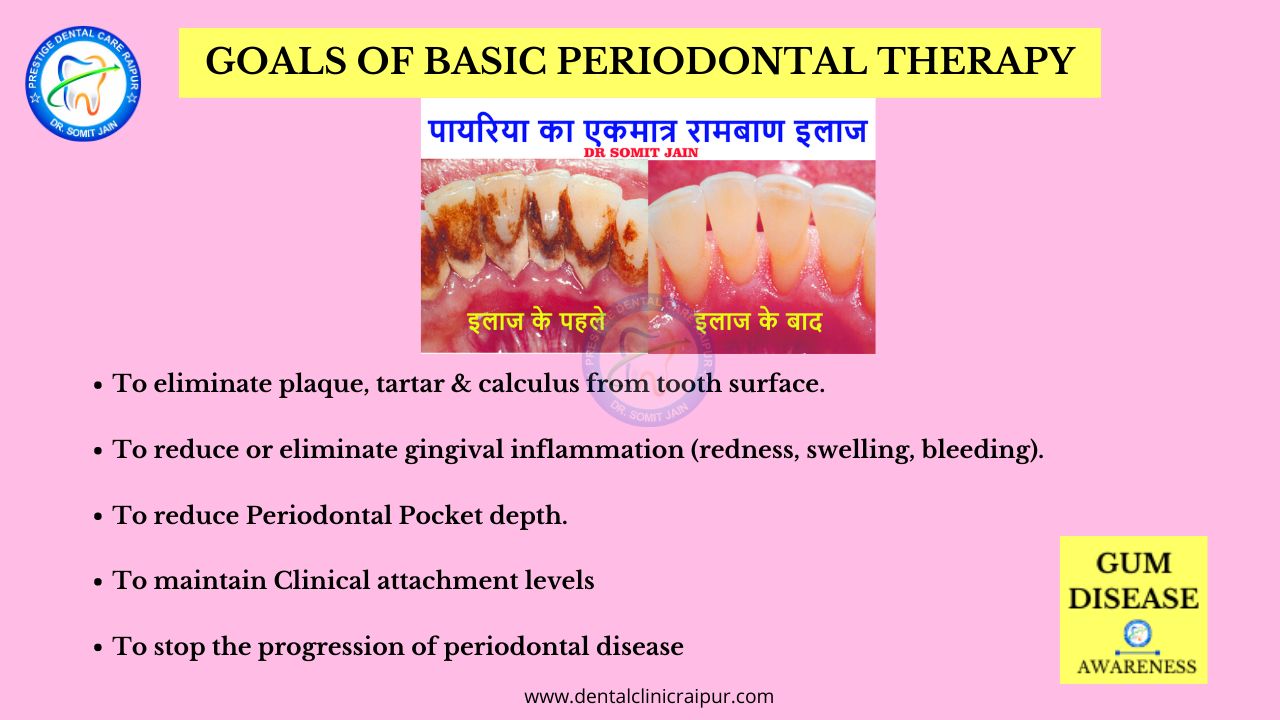
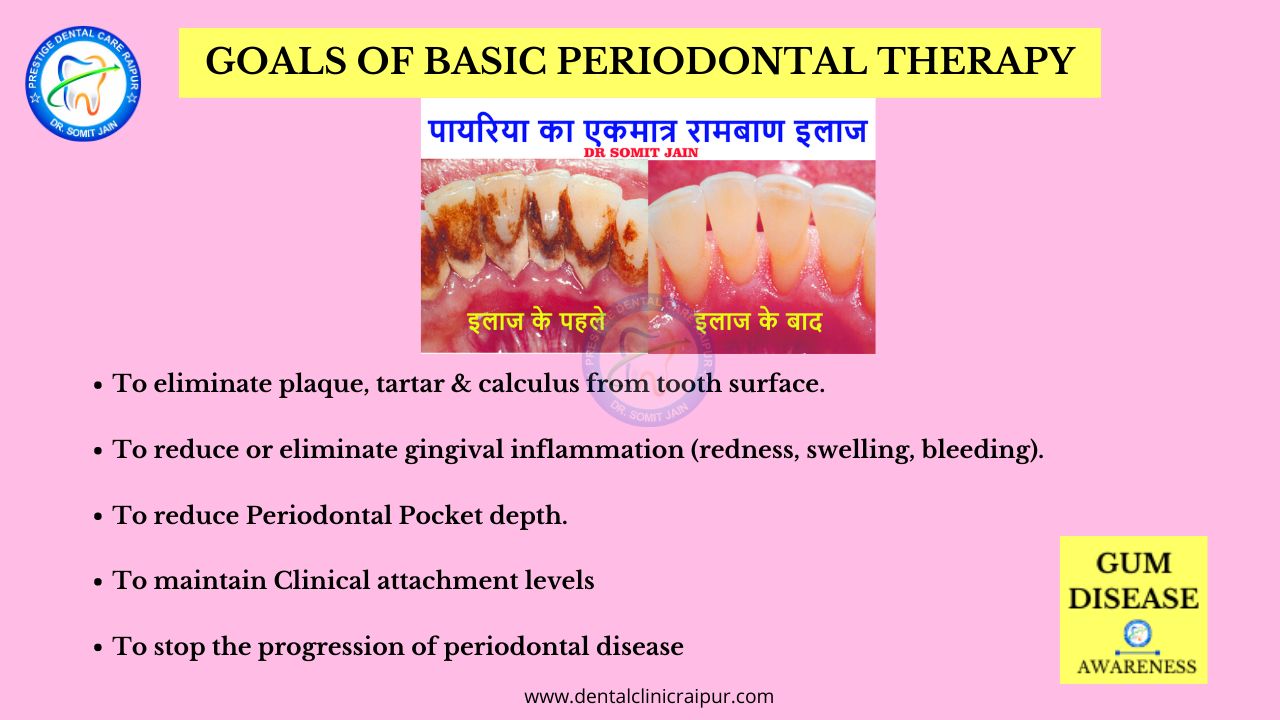
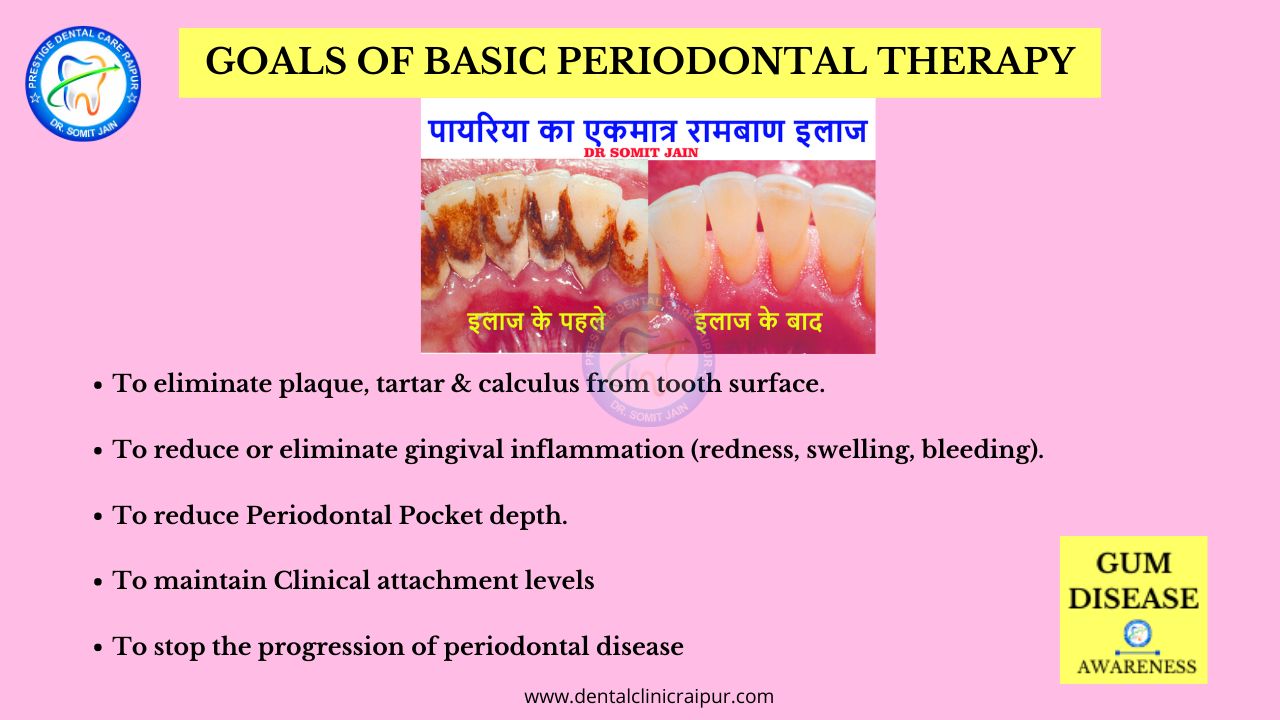
9#. How is periodontal disease or Gum disease treated?
- Gum (gingival) enlargement treatment
- How to treat (get rid of ) swollen gums?
- How to treat gingivitis and periodontitis?
- Severe gum disease treatment
- Inflamed gum pocket treatment
- Laser gum treatment near me
- Gingivectomy before and after
- Deep periodontal pocket treatment
- Deep cleaning teeth before and after pictures
- Periodontitis clinic treatment
- How to remove pyorrhea from teeth?



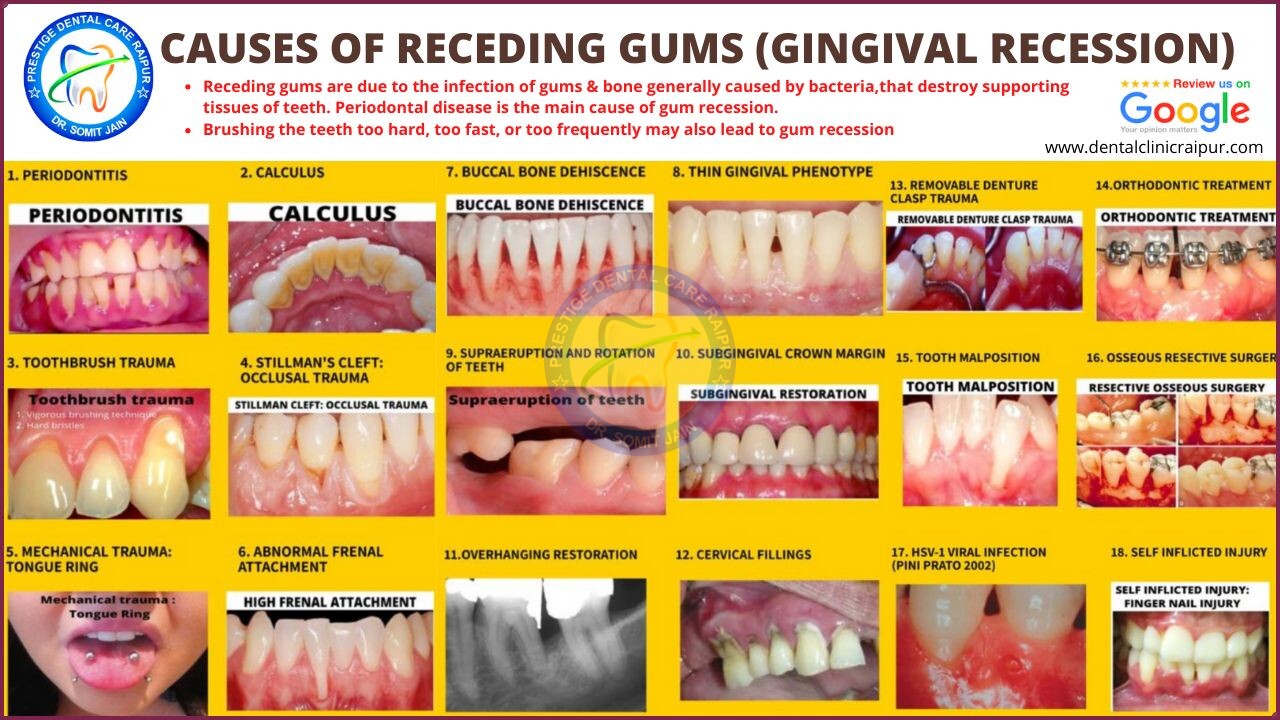
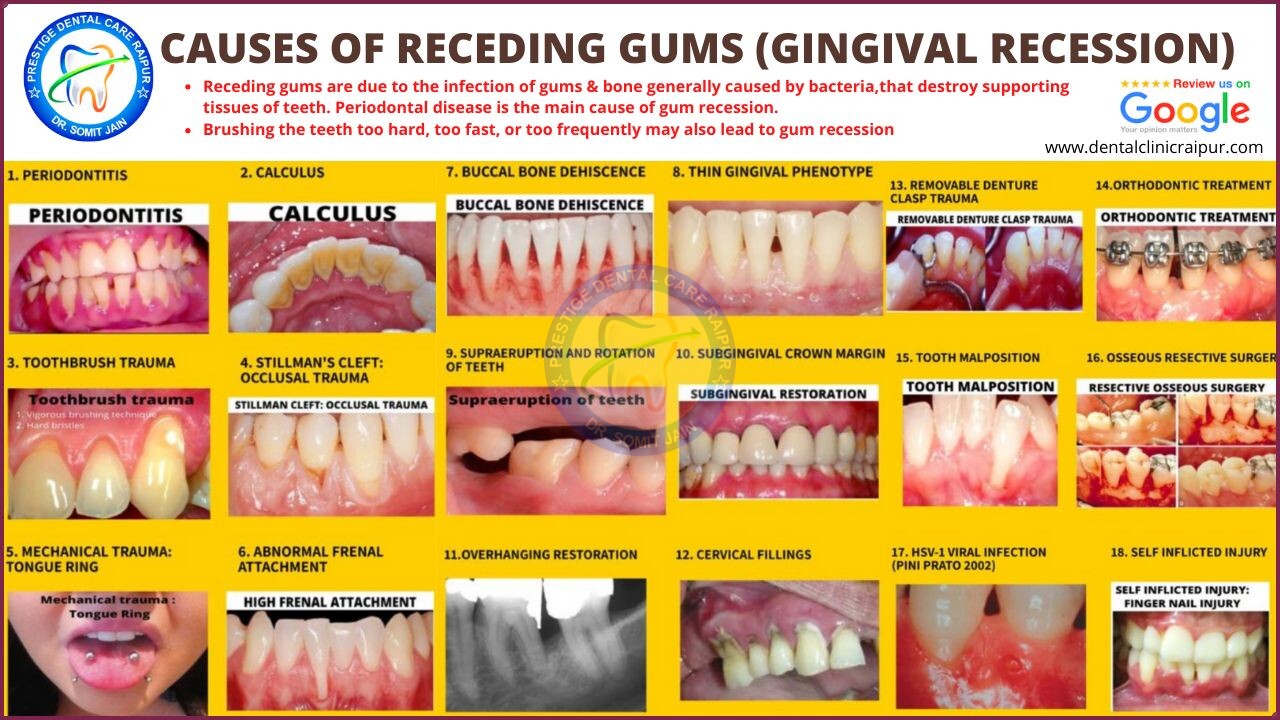
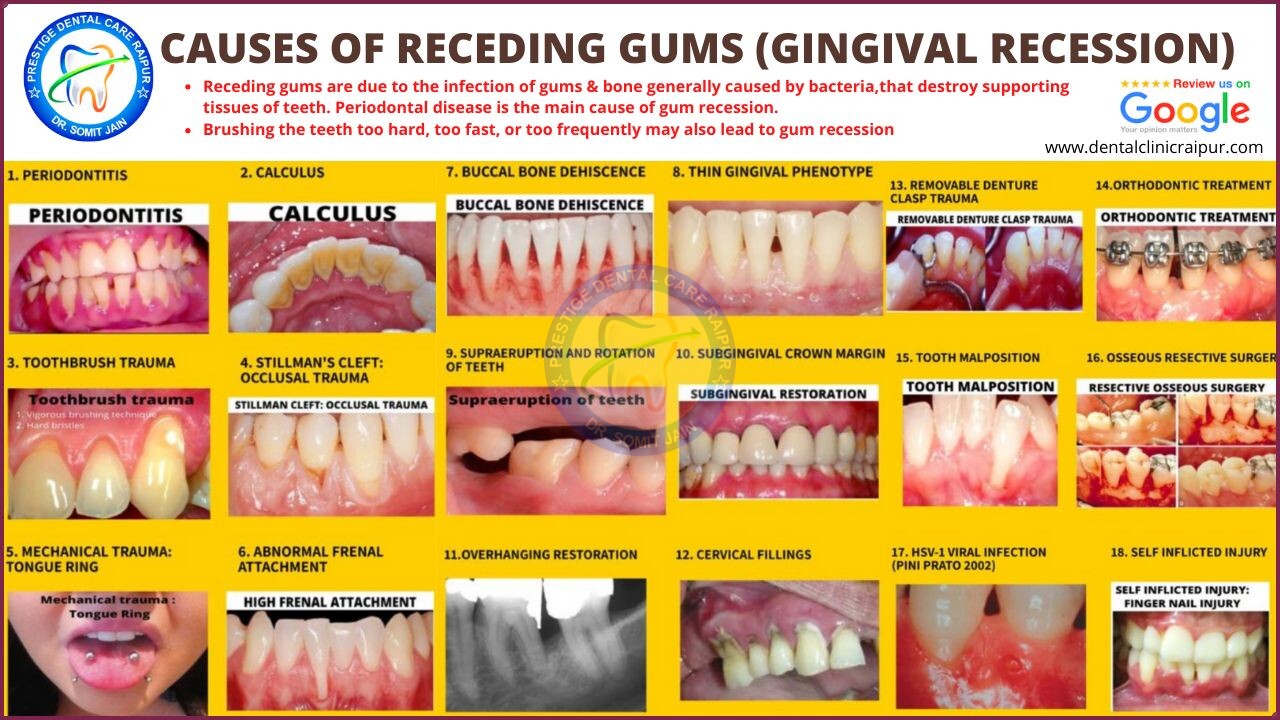
What are the causes of receding gums or gingival recession??
CAUSES OF RECEDING GUMS (GINGIVAL RECESSION)
- Receding gums are due to the infection of gums & bone generally caused by bacteria,that destroy supporting tissues of teeth. Periodontal disease is the main cause of gum recession.
- Brushing the teeth too hard, too fast, or too frequently may also lead to gum recession
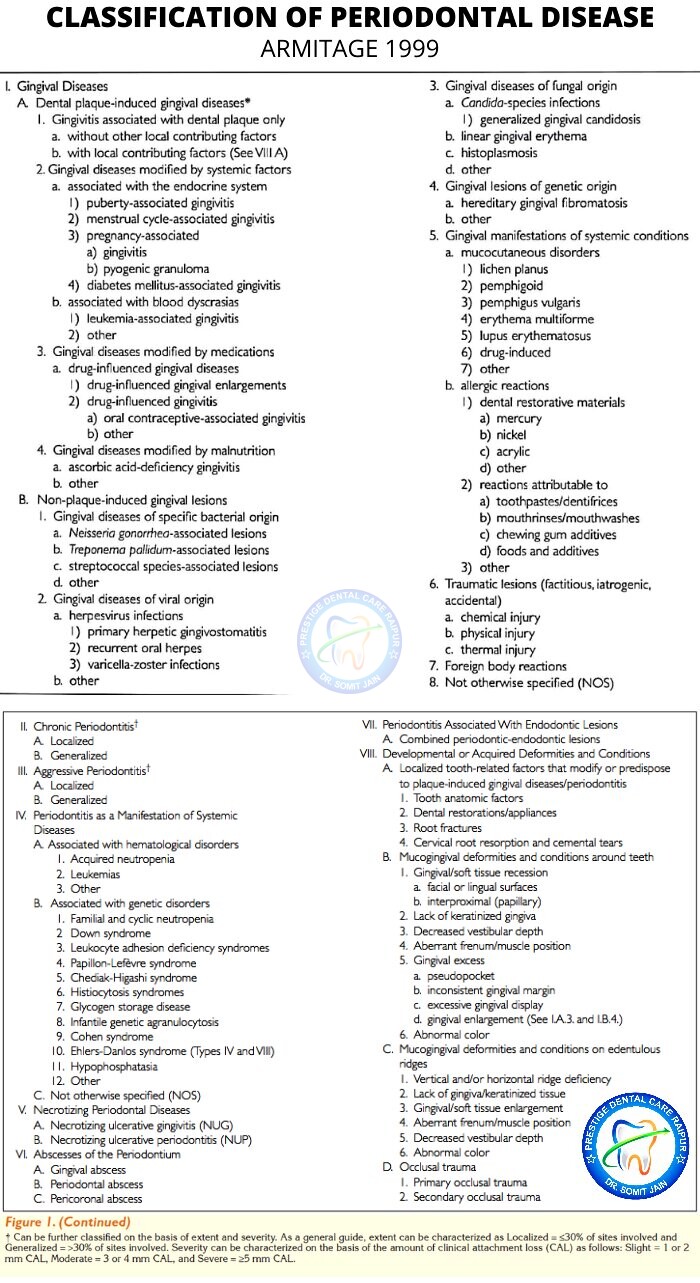
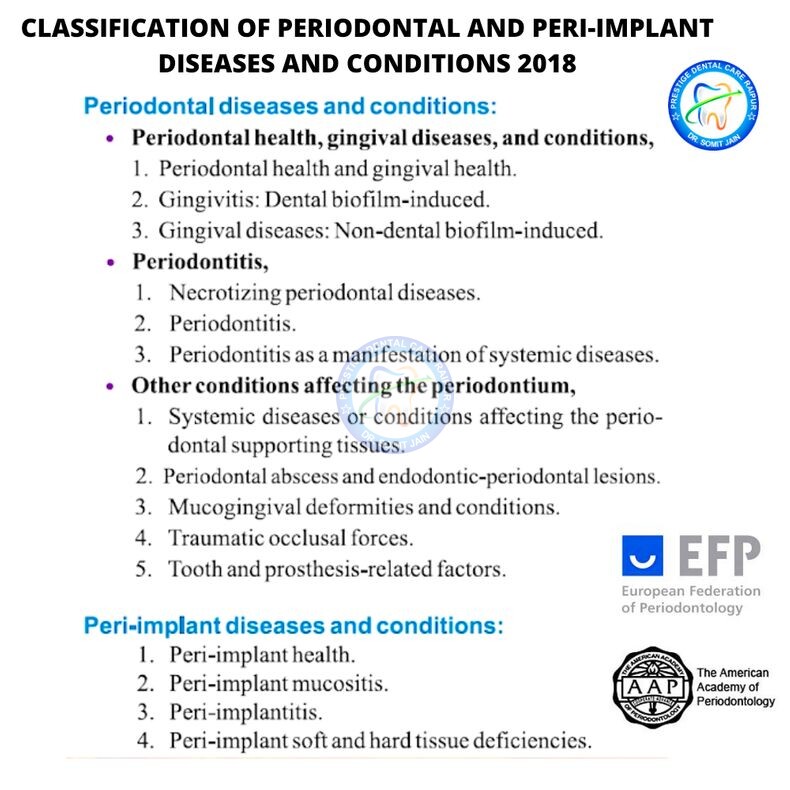
Key Elements in New classification of Periodontal Disease
DIAGNOSIS
Periodontal disease is a silent, mostly painless, condition, so it commonly reaches advanced degrees of severity before it is detected and treatment is started.
Manifestations of chronic periodontitis include redness, swelling and recession of the gingiva, bleeding of the affected gingival area on probing and increased tooth mobility due to loss of supportive structures. Tissue loss results in the
formation of periodontal pockets and bone loss, which are the hallmarks of the disease.
A diagnosis is made mostly based on clinical parameters that include clinical attachment level (a measure of the loss of soft and hard tissue), bleeding on
probing, probing depth (the depth of the pocket) and radiographic findings (to assess bone loss).
Prevention is typically achieved with self‑performed (daily) and professional (bi-annually) oral hygiene.
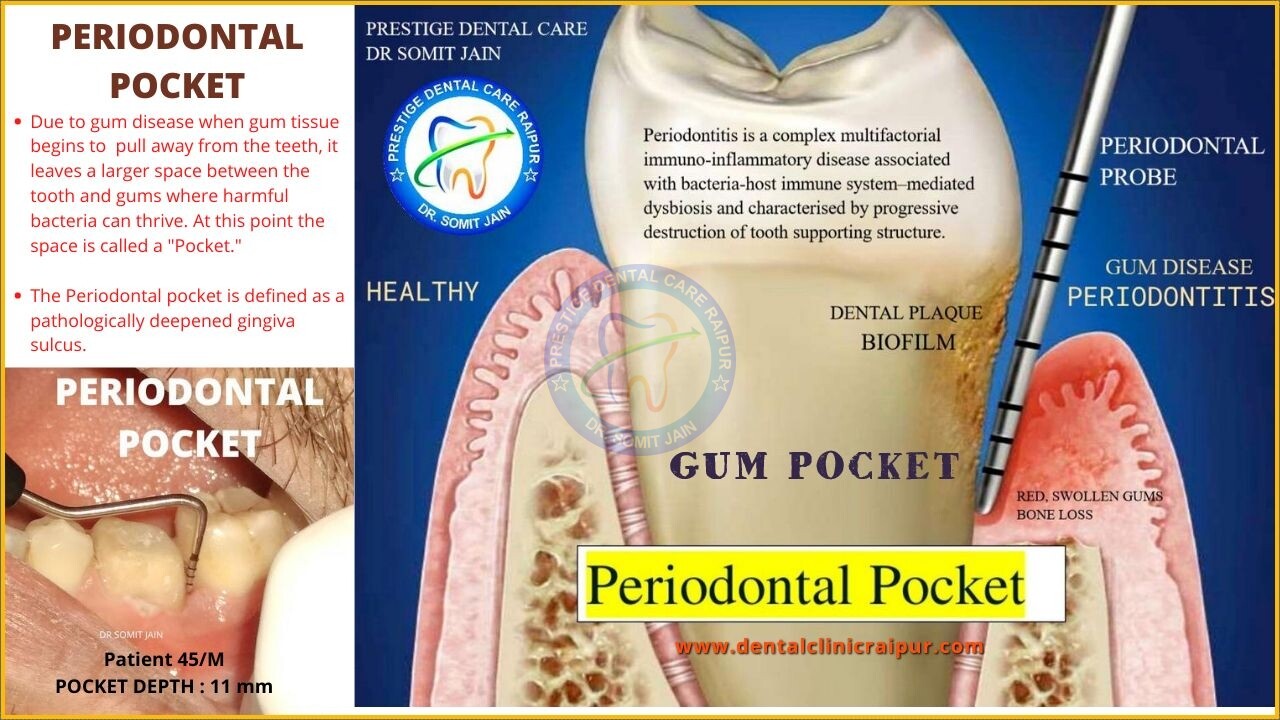
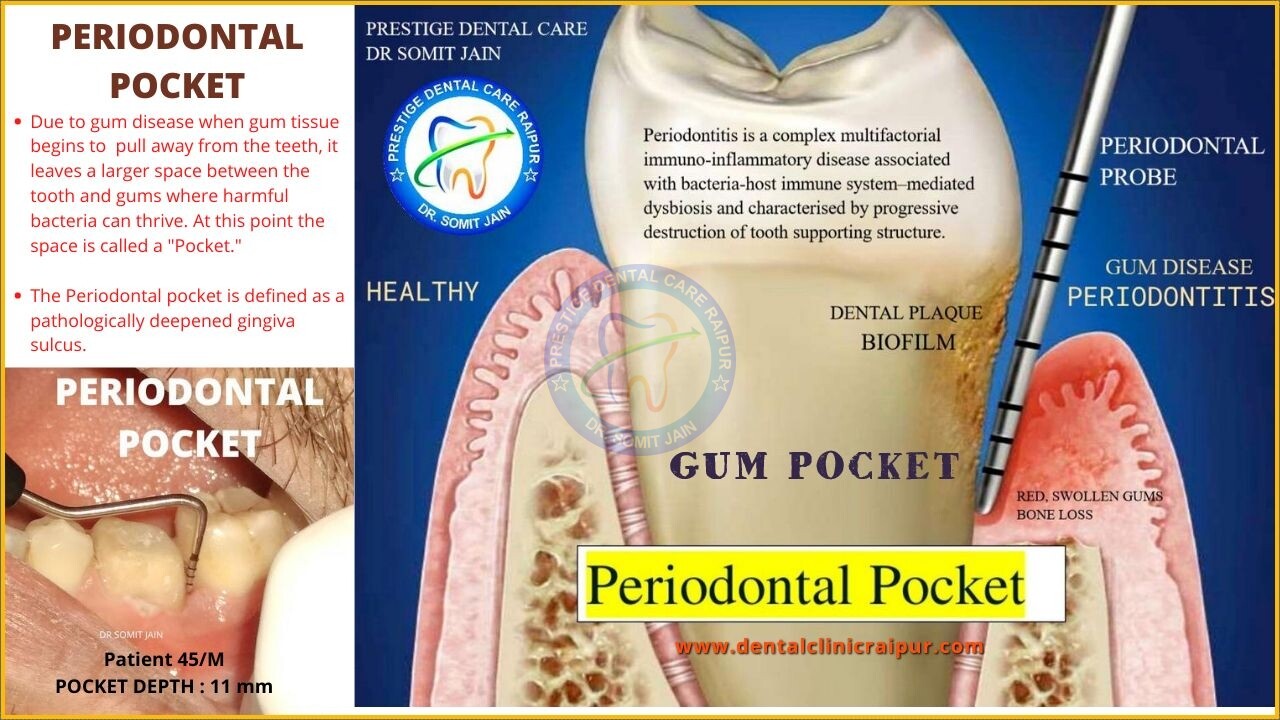
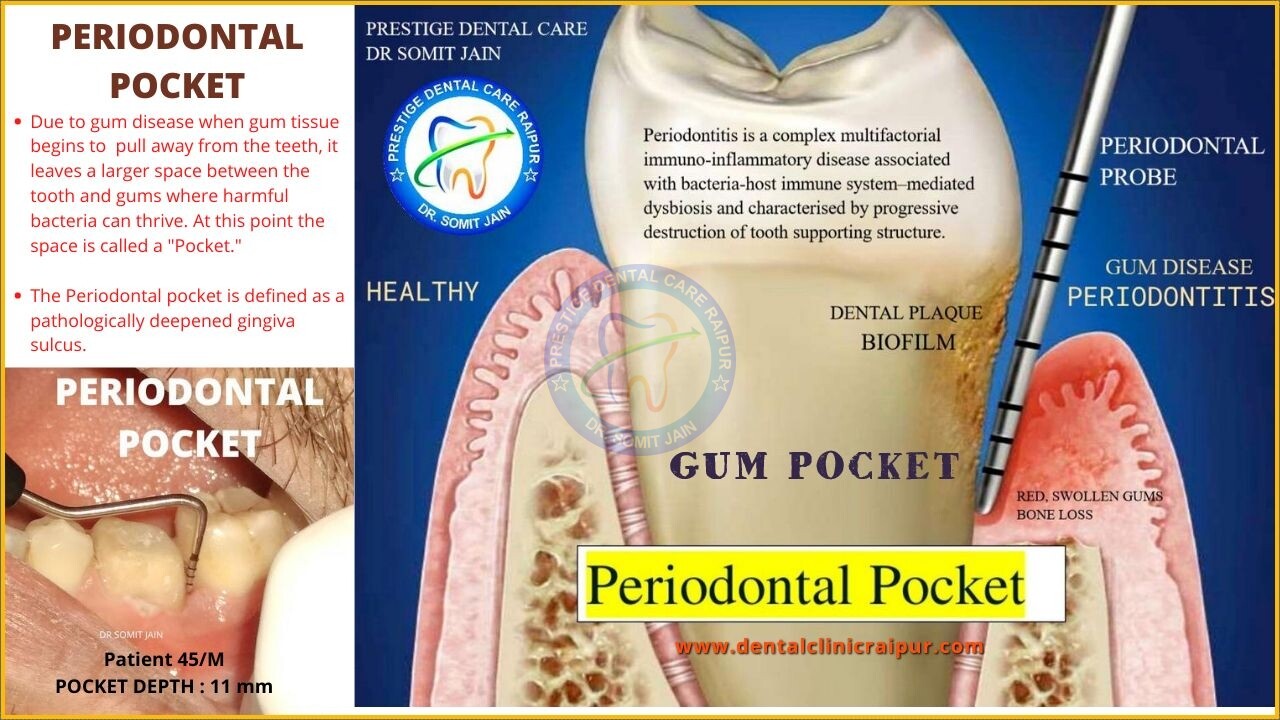
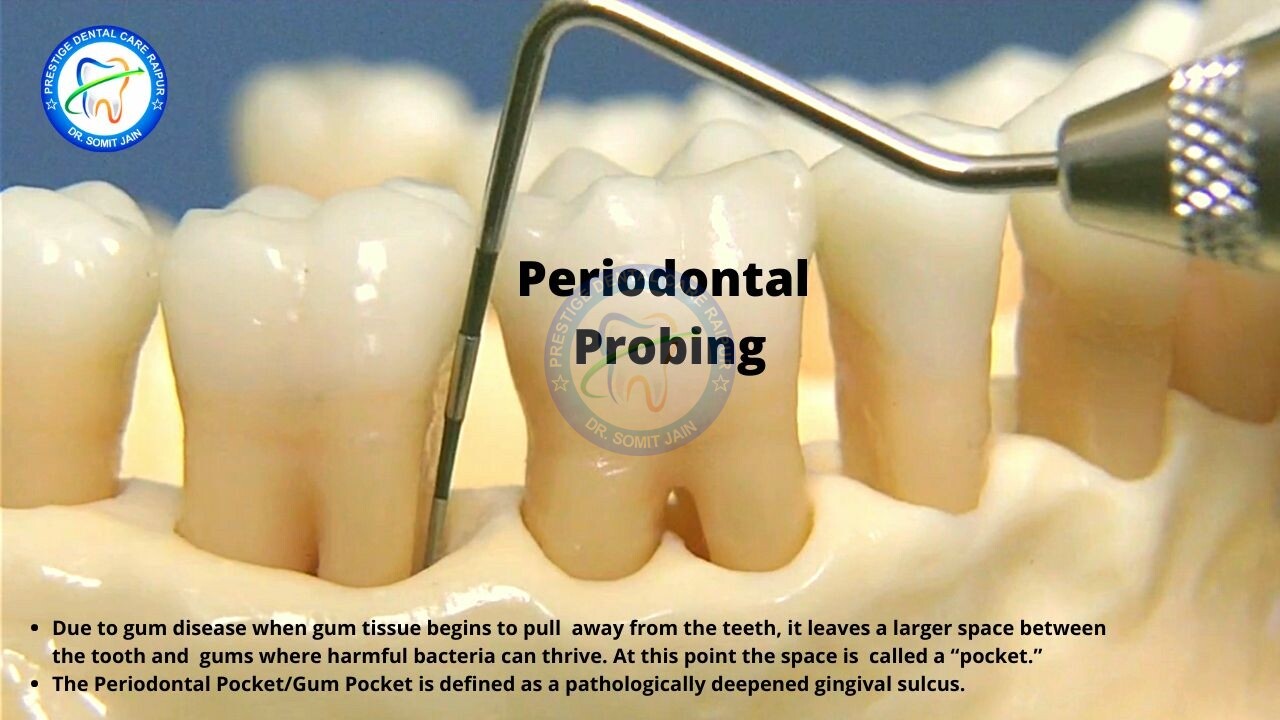
What is Periodontal Pocket or a Gum Pocket??
CLINICAL DIAGNOSIS: PERIODONTAL POCKET PROBING
- Due to gum disease when gum tissue begins to pull away from the teeth, it leaves a larger space between the tooth and gums where harmful bacteria can thrive. At this point the space is called a “pocket.”
- The Periodontal pocket is defined as a pathologically deepened gingiva sulcus.
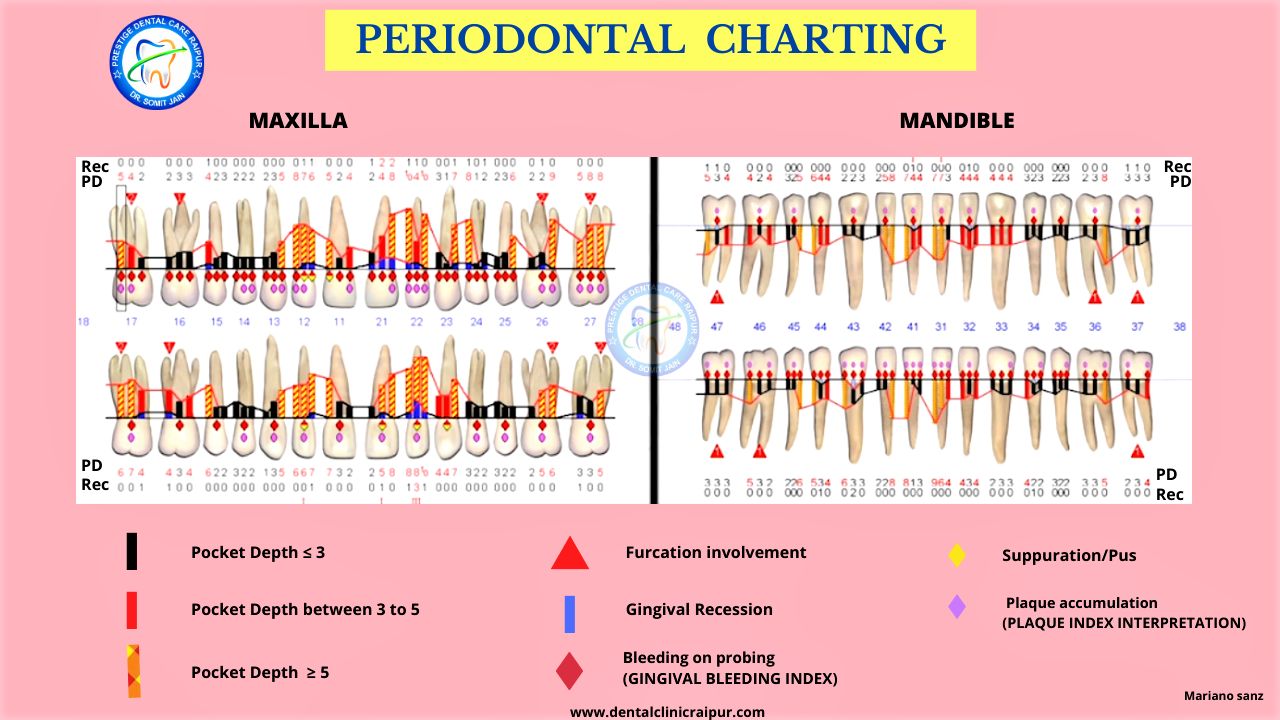
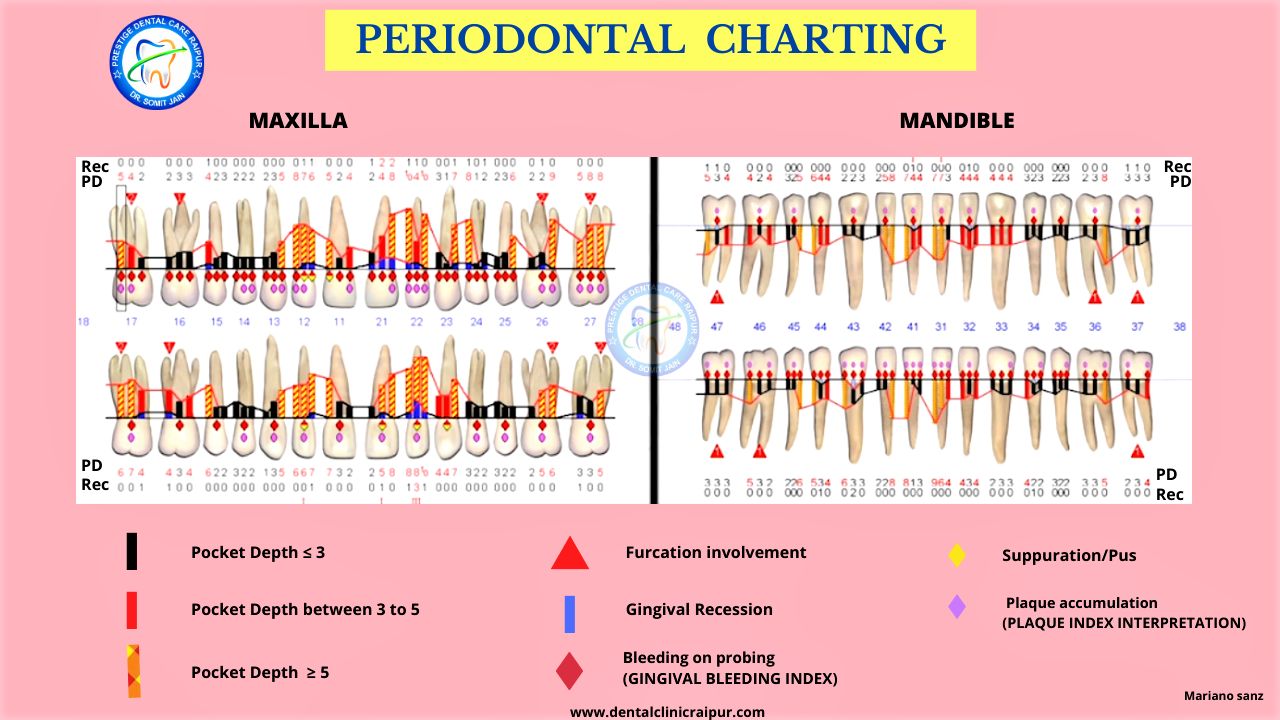
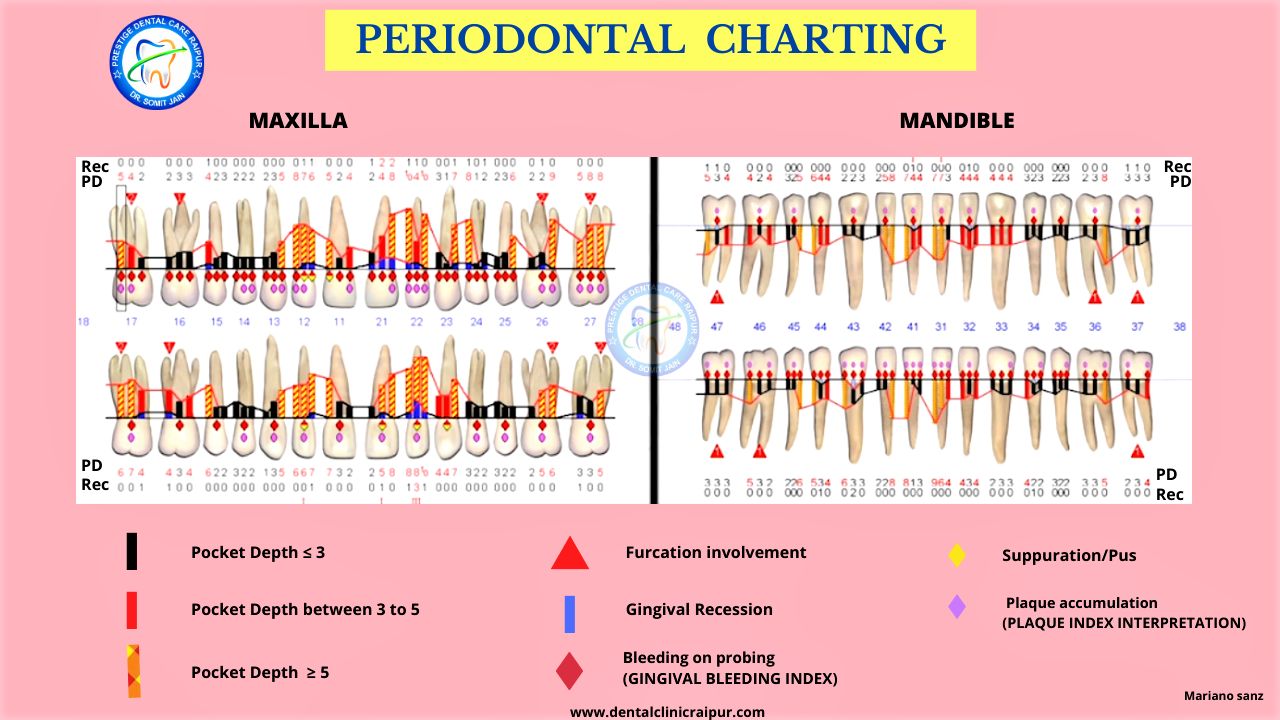
PERIODONTAL CHARTING
Periodontal charting refers to a chart utilized by a Periodontist or Gum Specialist to evaluate and record gingiva, alveolar bone and overall oral conditions relating to gum health or disease.
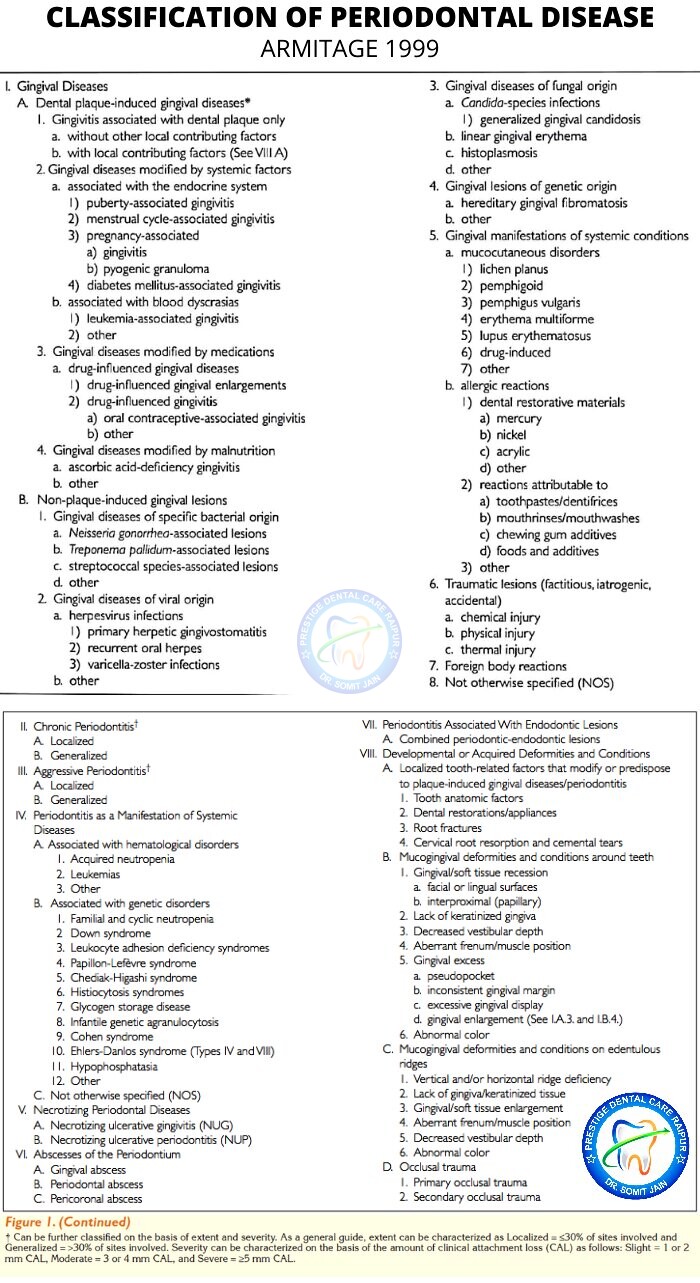
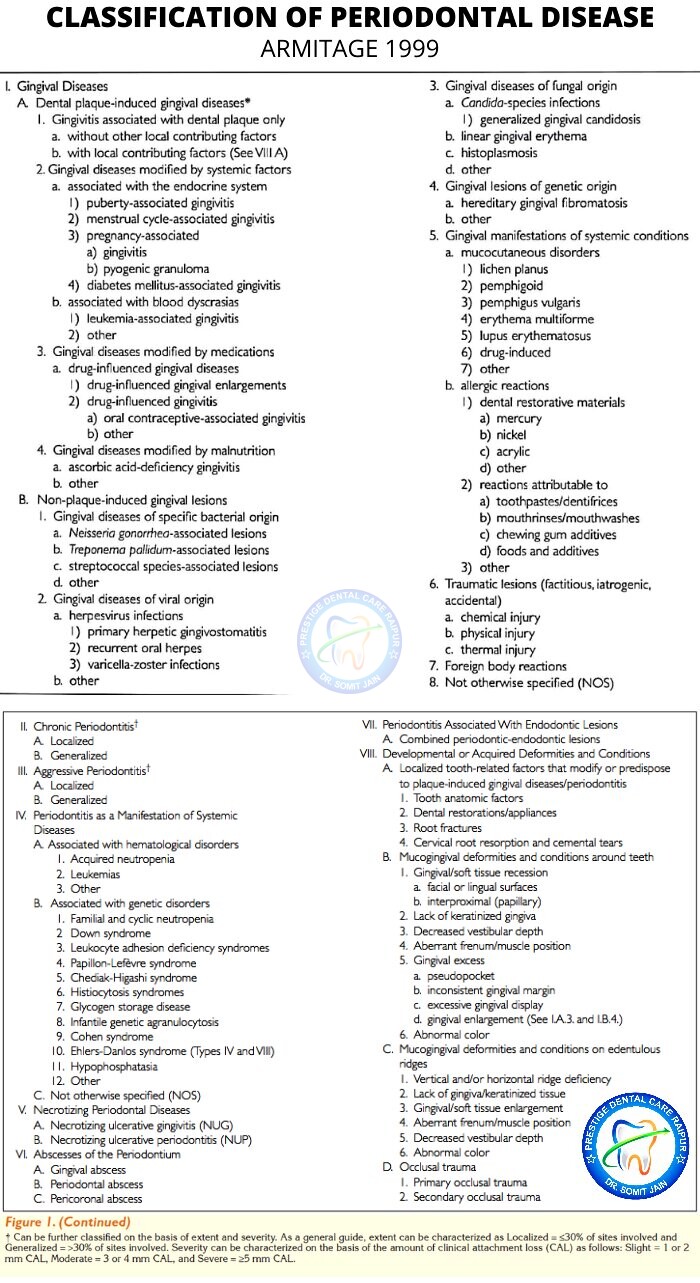
CLASSIFICATION OF PERIODONTAL DISEASE 1999
7#. How does Periodontist vs Dentist diagnose Gum disease?



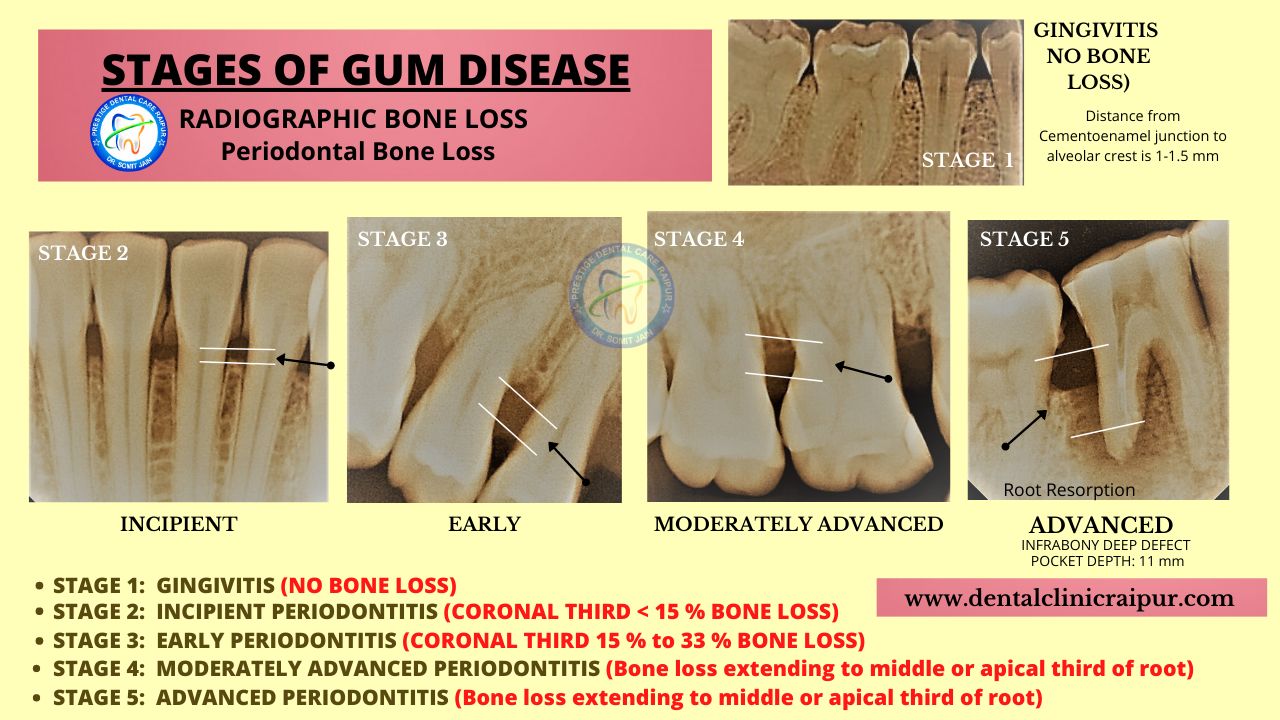
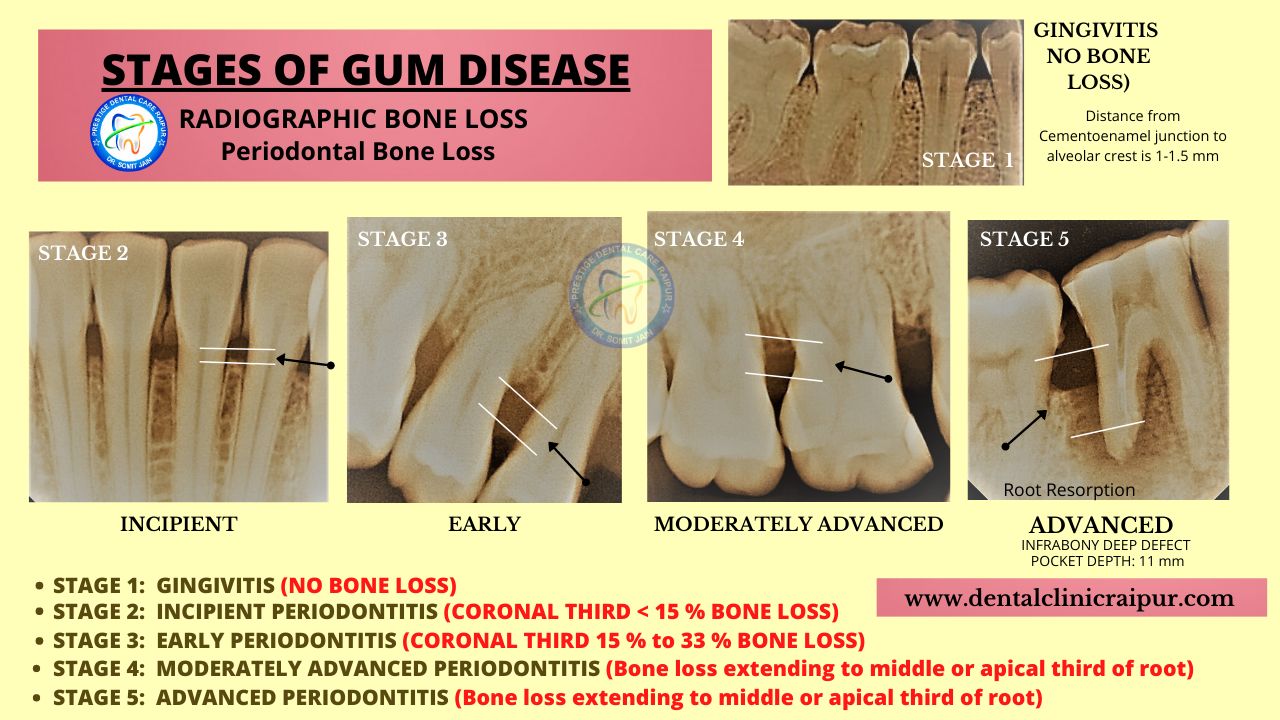
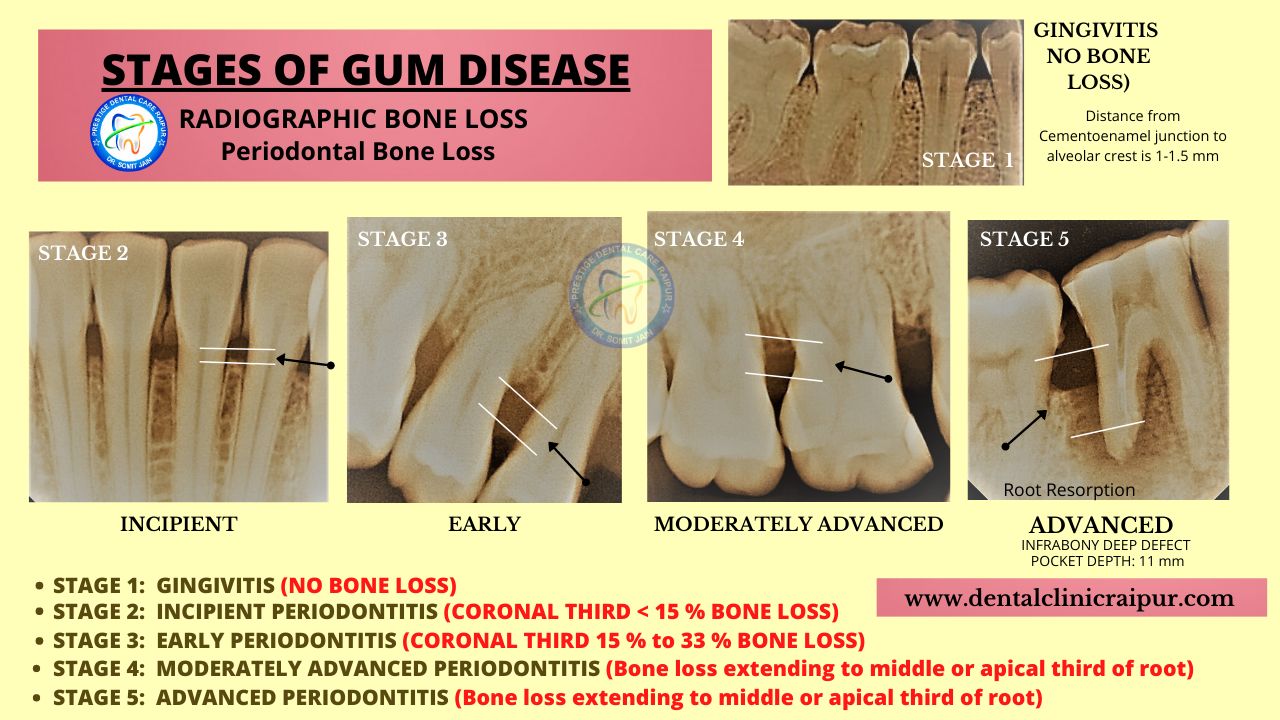
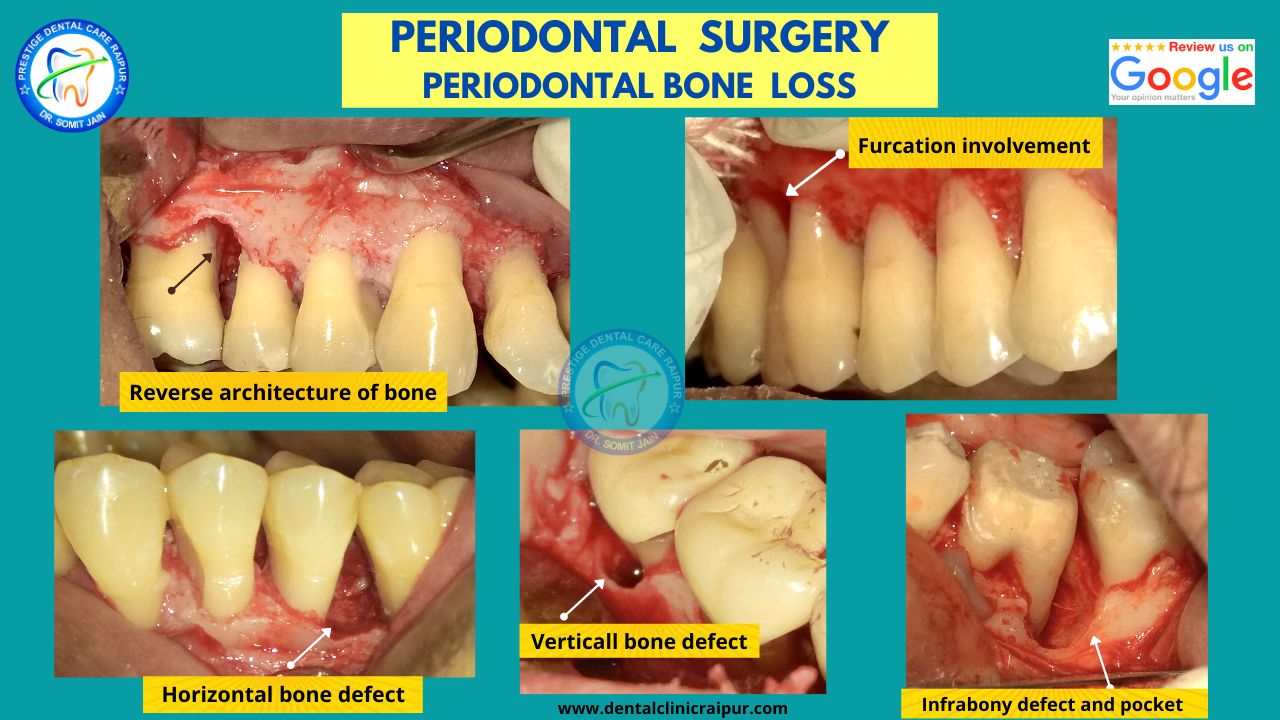
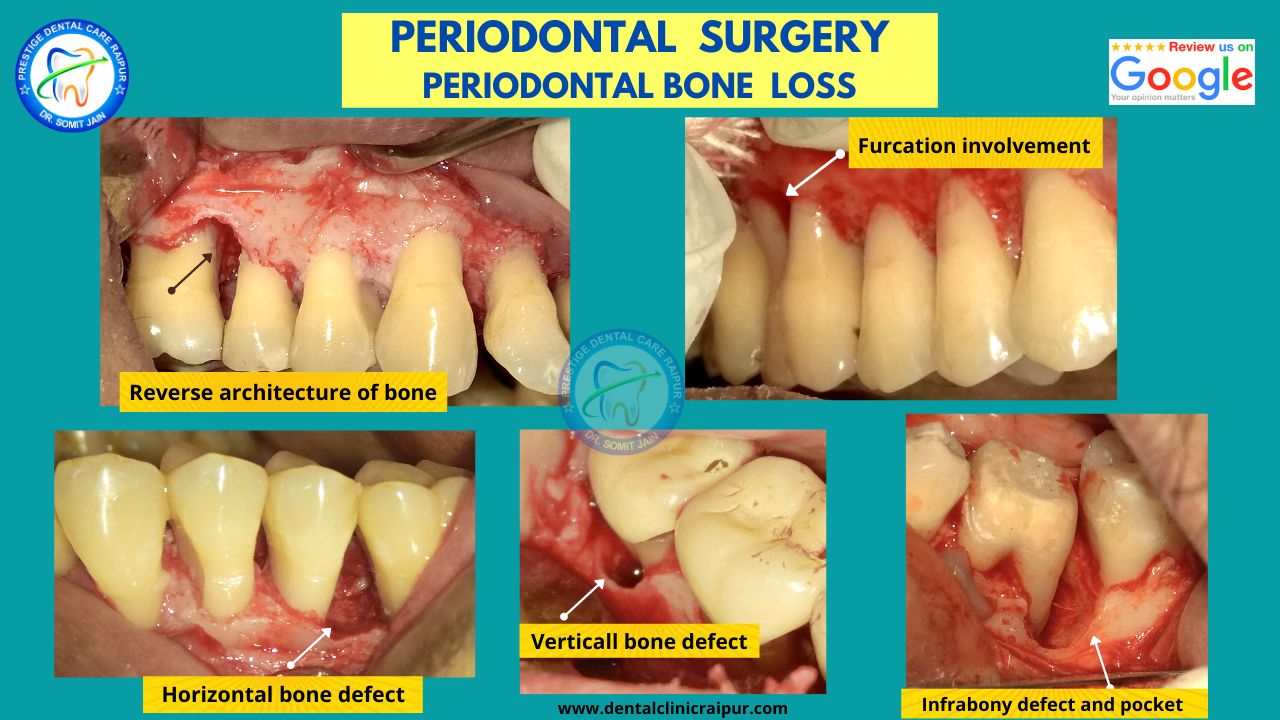
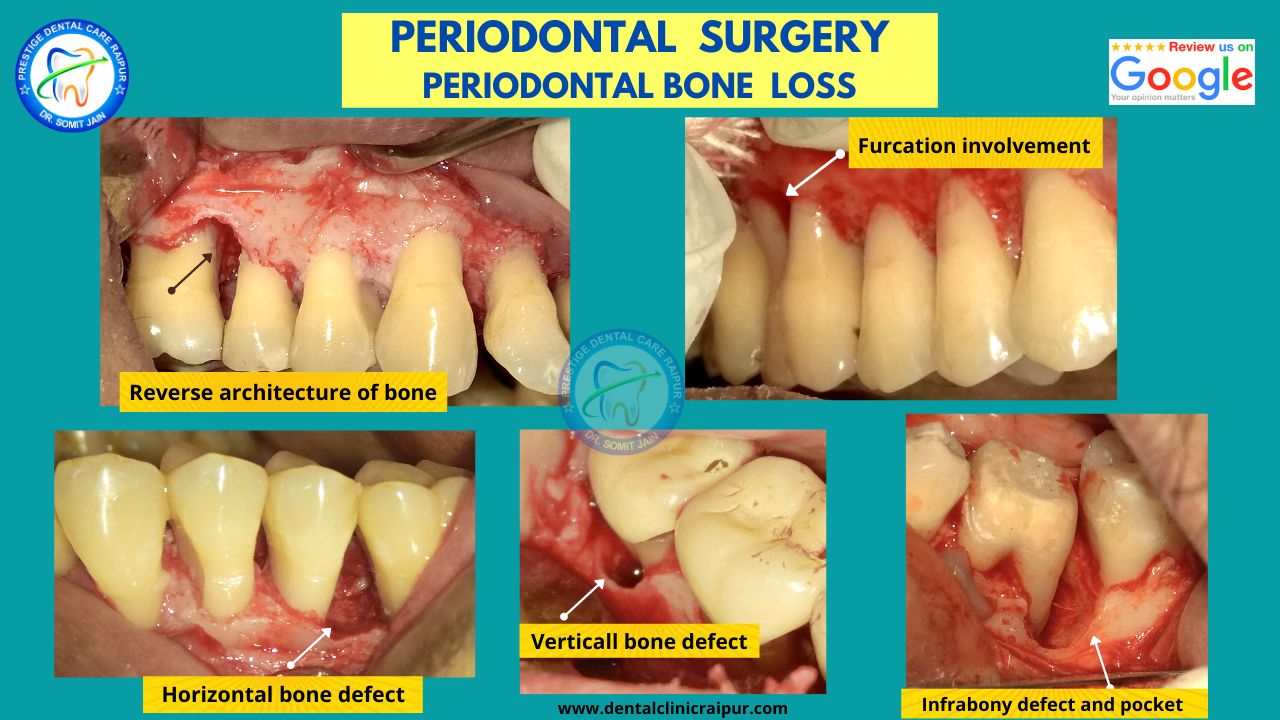
PERIODONTAL BONE LOSS : RADIOGRAPHIC DIAGNOSIS



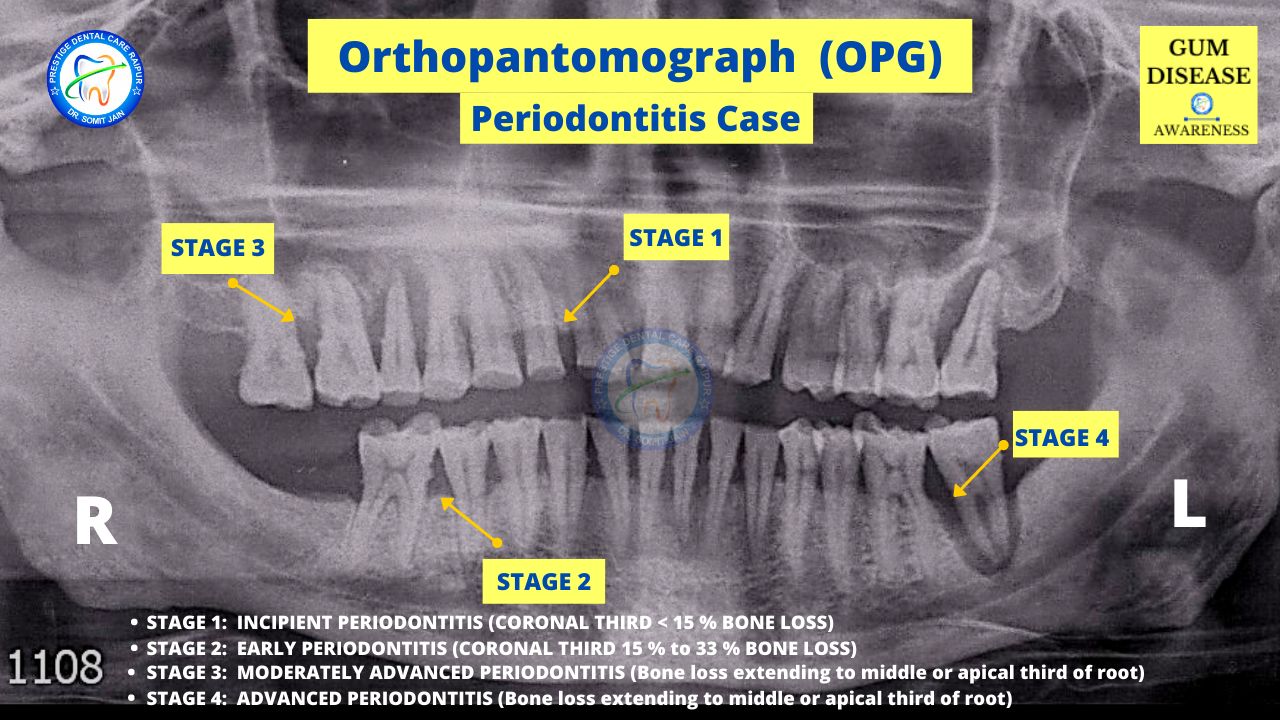
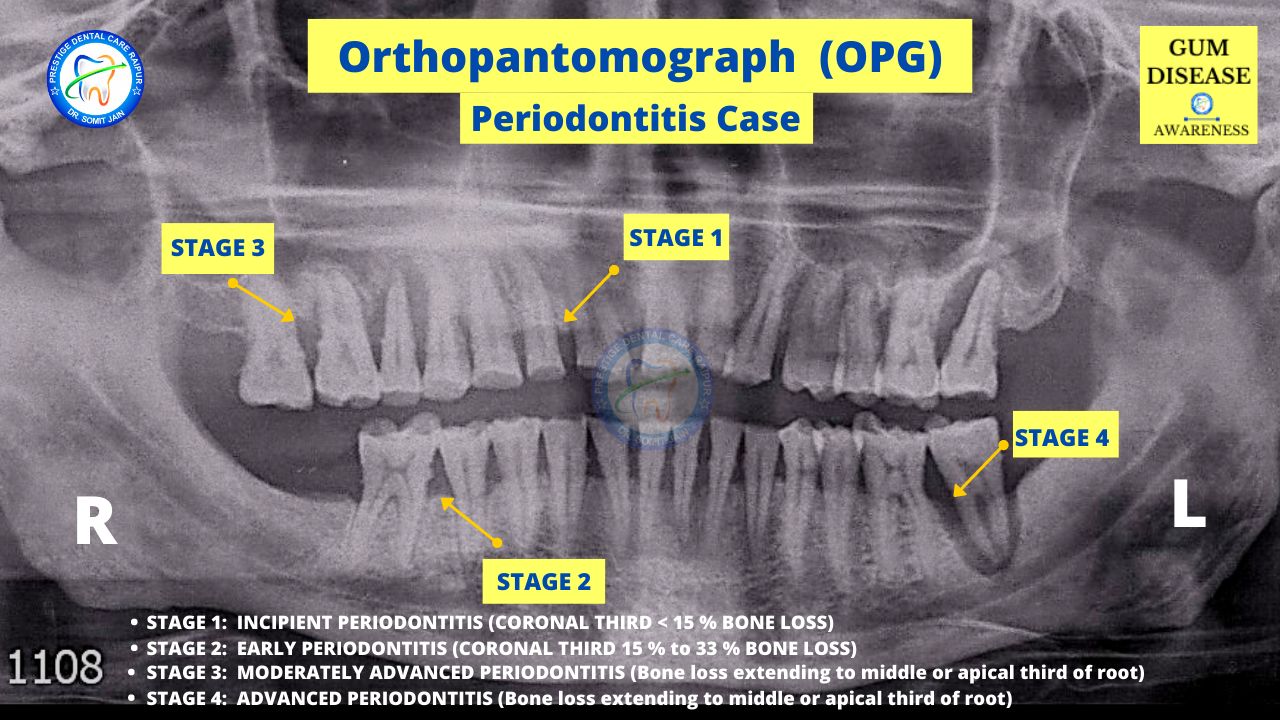
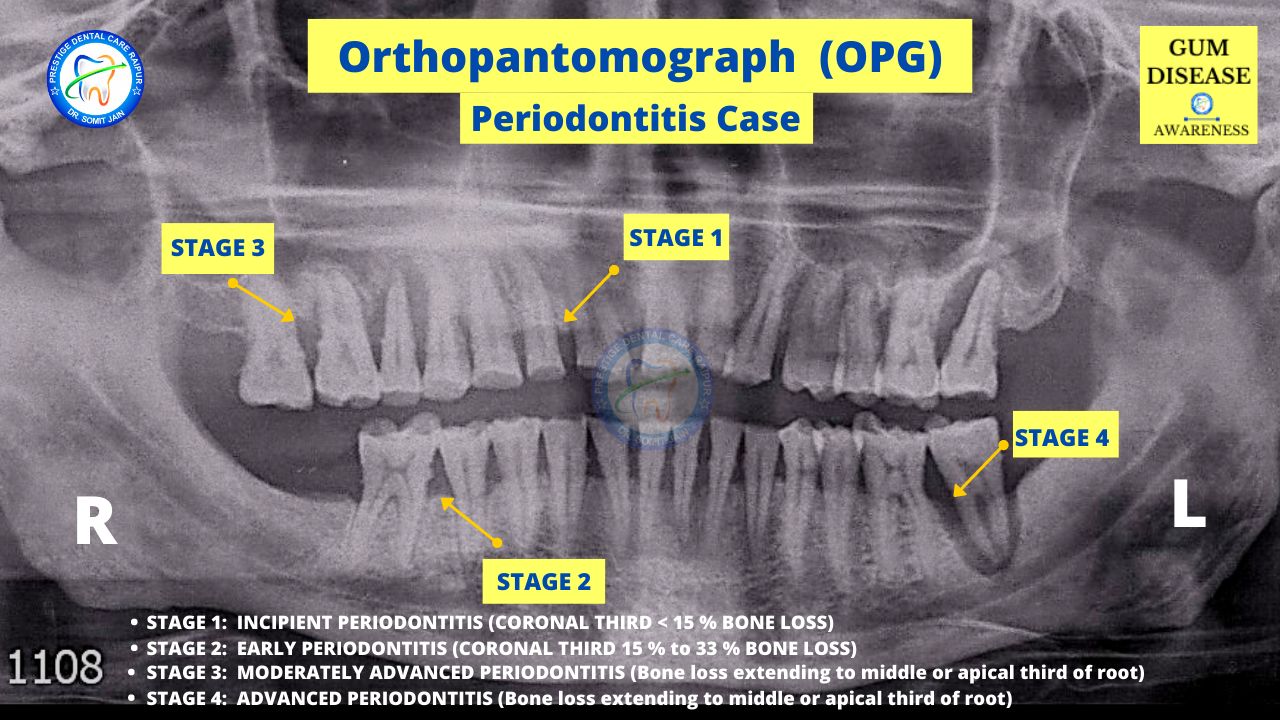
PERIODONTAL BONE LOSS



STAGES OF GUM DISEASE/PERIODONTAL DISEASE
GINGIVITIS VS PERIODONTITIS
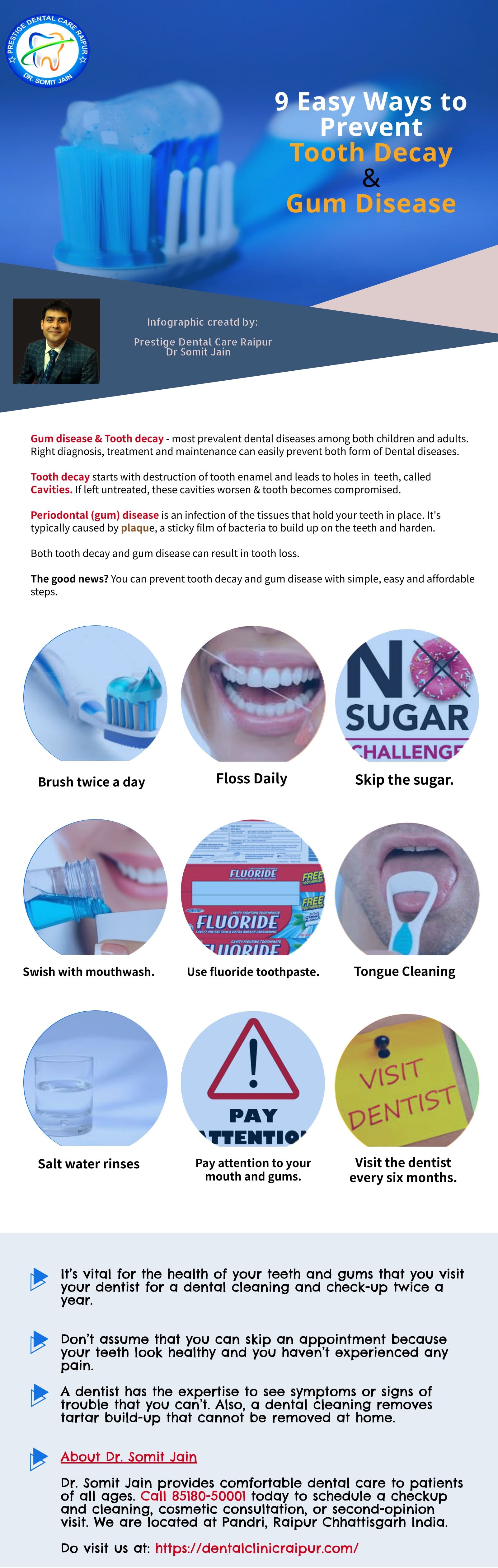
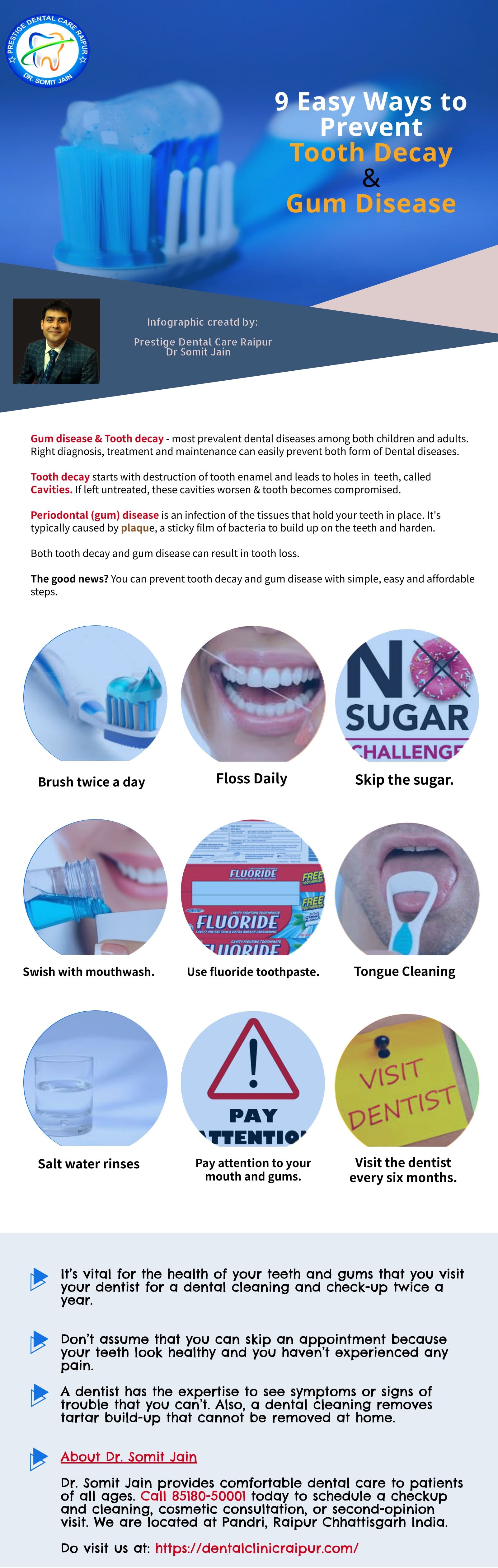
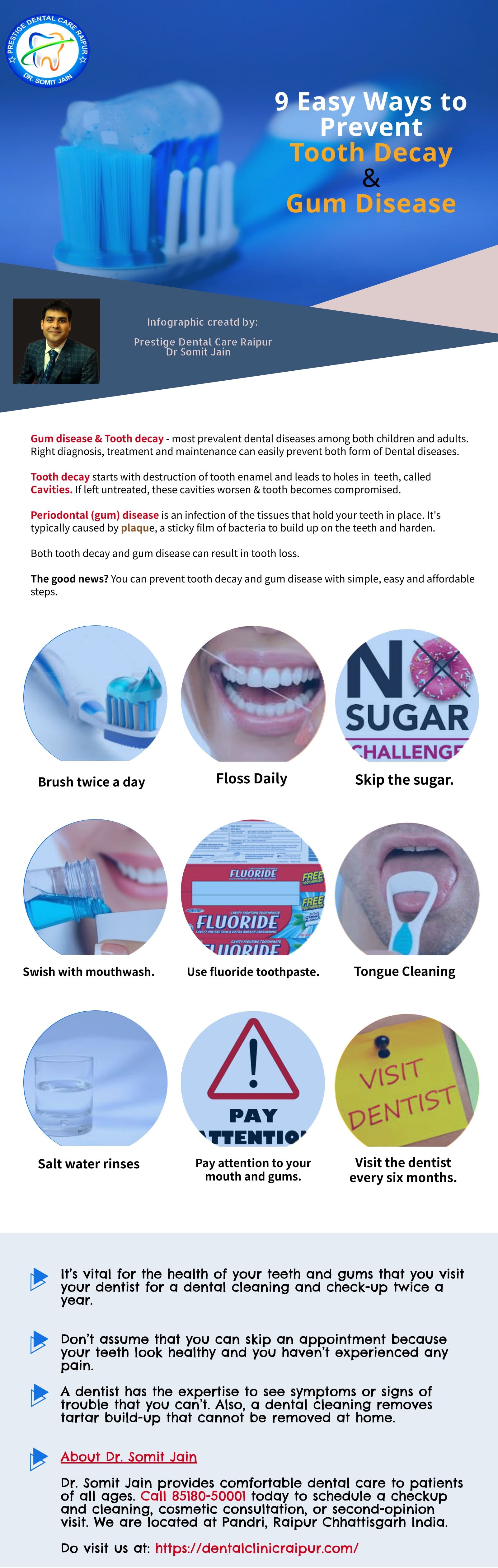
8#. How can Gum disease be prevented?
- Brush your teeth at least twice a day. If possible, clean oral cavity after each meal.
- One of the best things you can do is swish warm, salty water around in your mouth
- Electric toothbrush to maximize your cleaning potential.
- The Waterpik Water Flosser is the only Water Flosser to earn the American Dental Association (ADA) Seal of acceptance.
- Make sure your toothbrush has soft or extra-soft bristles.
- Replace your toothbrush every three months.
- Floss daily
- Interdental brushes for orthodontic cases and natural gaps between teeth.
- Use a natural mouthwash.
- Visit your dentist at least once a year.
- Refrain from smoking or chewing tobacco.
- Limit sugar
- Oil pulling
- Exposing teeth to salt or baking soda could erode the tooth’s surface enamel over time so try to avoid that.
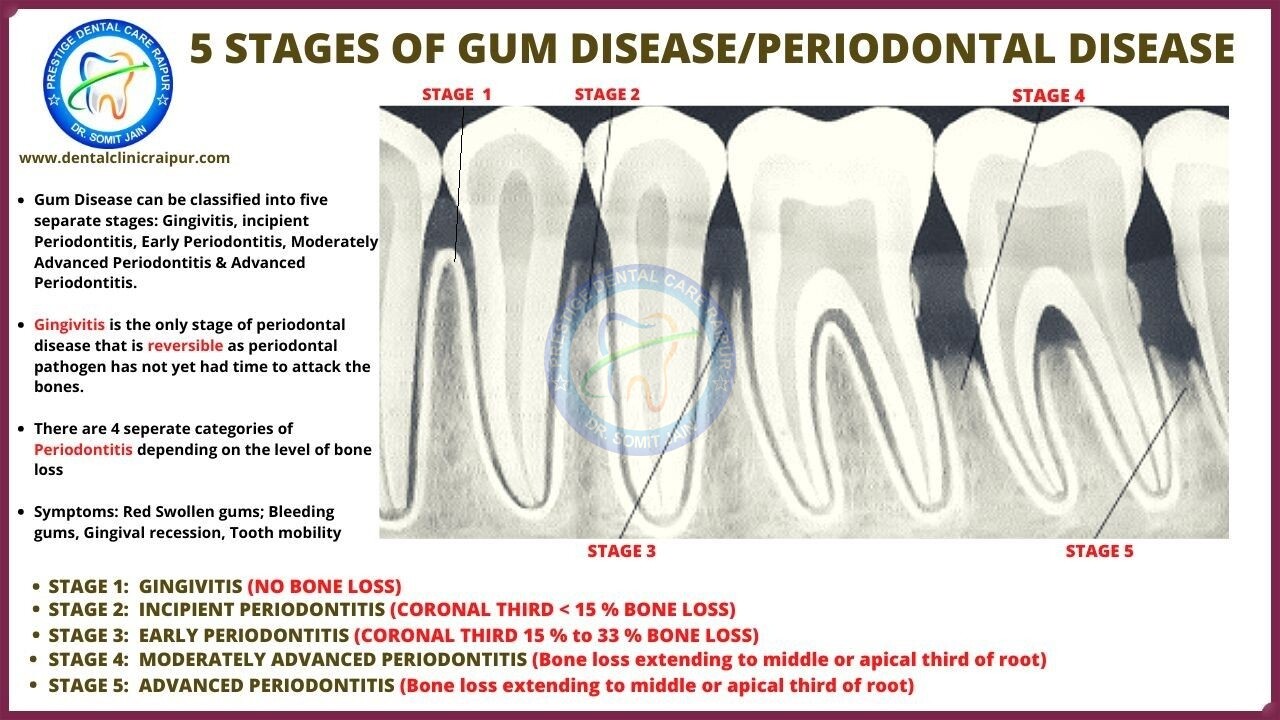
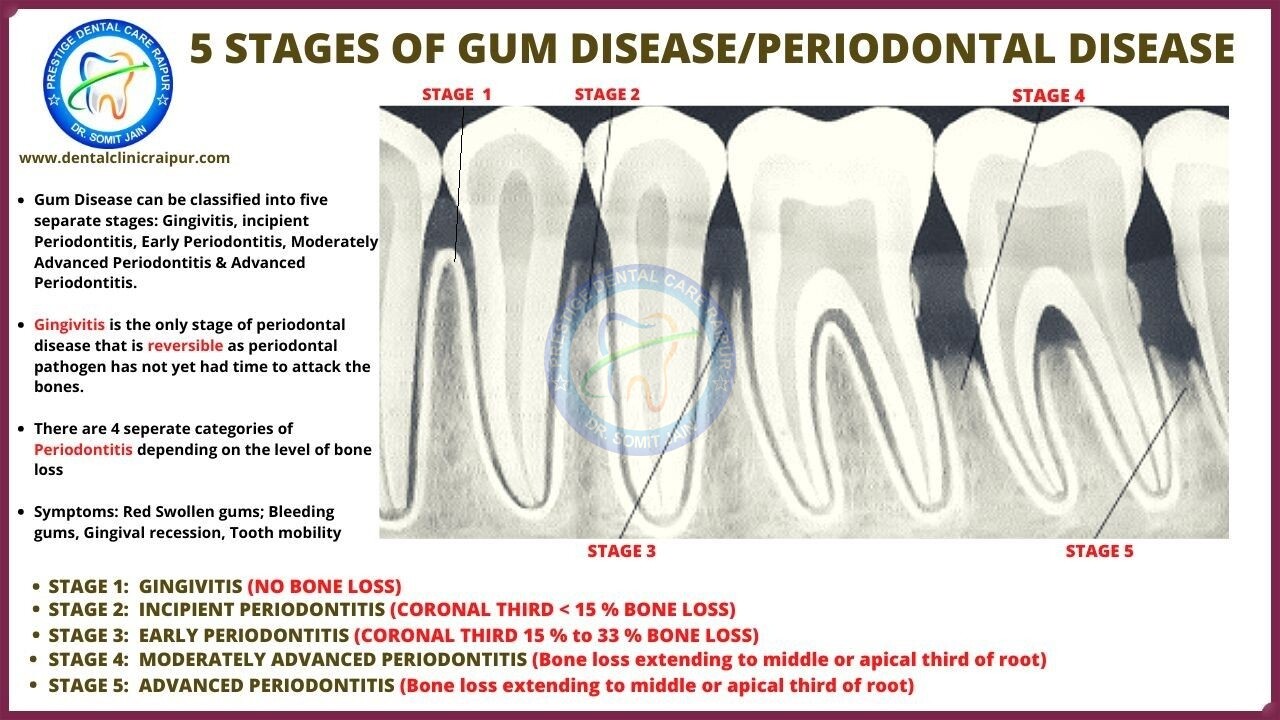
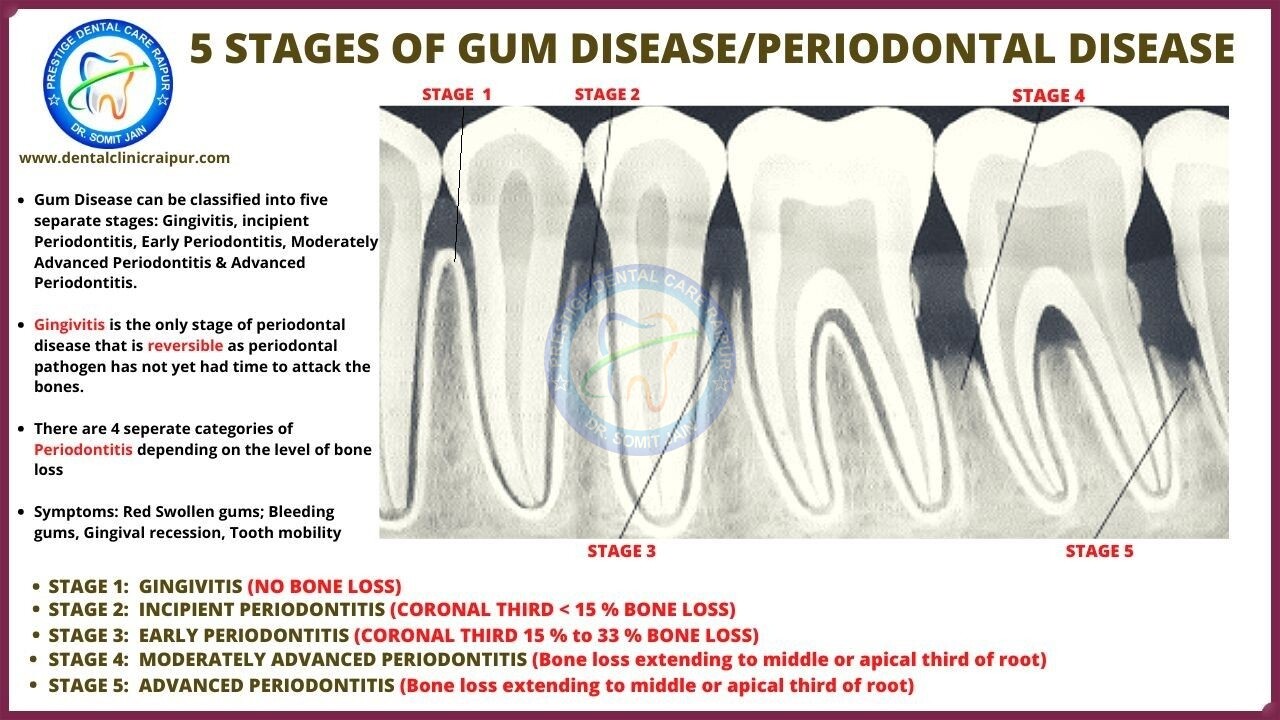
What are the 5 stages of Gum Disease/Periodontal Disease
- Gum Disease can be classified into five separate stages: Gingivitis, incipient Periodontitis, Early Periodontitis, Moderately Advanced Periodontitis & Advanced Periodontitis.
- Gingivitis is the only stage of periodontal disease that is reversible as periodontal pathogen has not yet had time to attack the bones.
- There are 4 seperate categories of Periodontitis depending on the level of bone loss
- Symptoms: Red Swollen gums; Bleeding gums, Gingival recession, Tooth mobility
- STAGE 1: GINGIVITIS (NO BONE LOSS)
- STAGE 2: INCIPIENT PERIODONTITIS (CORONAL THIRD < 15 % BONE LOSS)
- STAGE 3: EARLY PERIODONTITIS (CORONAL THIRD 15 % to 33 % BONE LOSS)
- STAGE 4: MODERATELY ADVANCED PERIODONTITIS (Bone loss extending to middle or apical third of root)
- STAGE 5: ADVANCED PERIODONTITIS (Bone loss extending to middle or apical third of root)
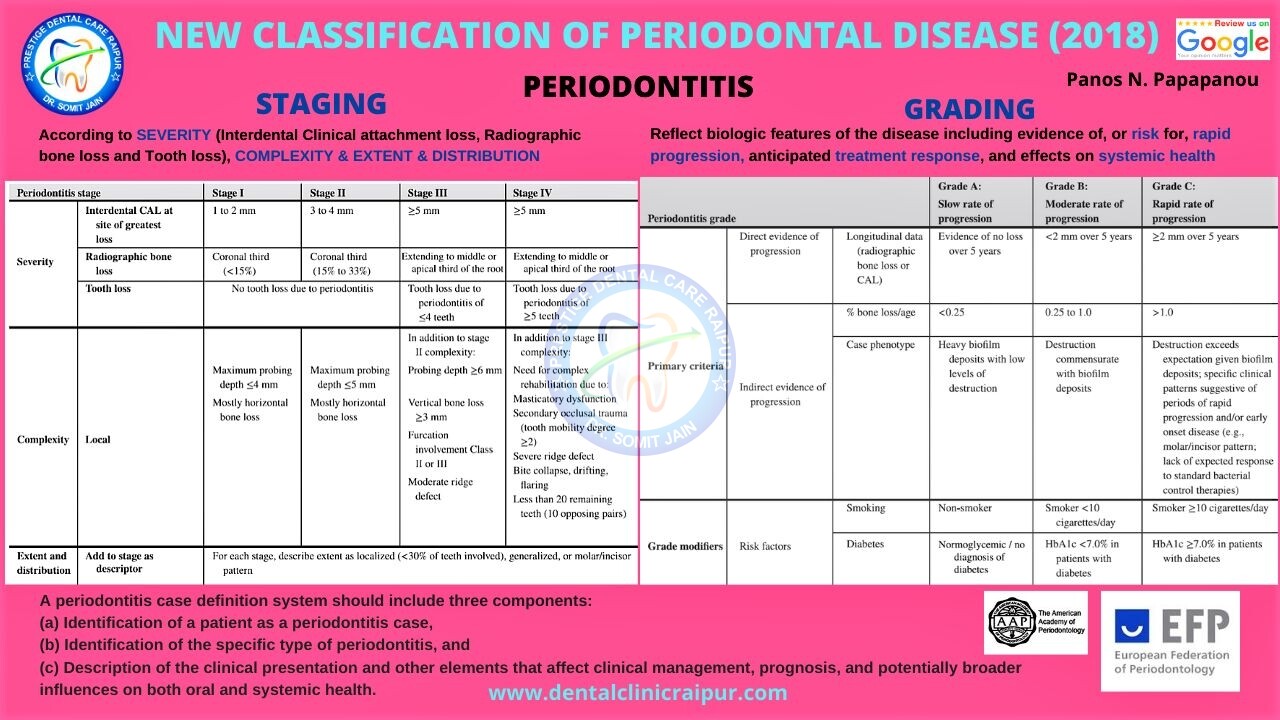
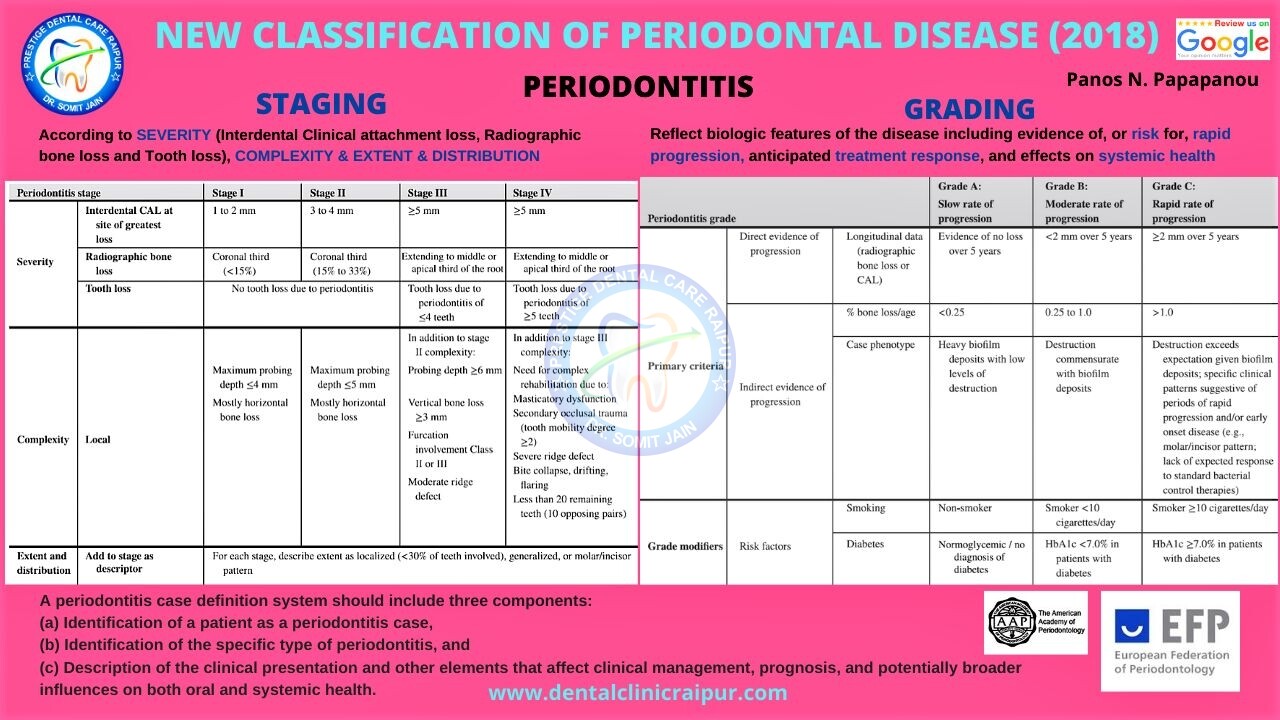
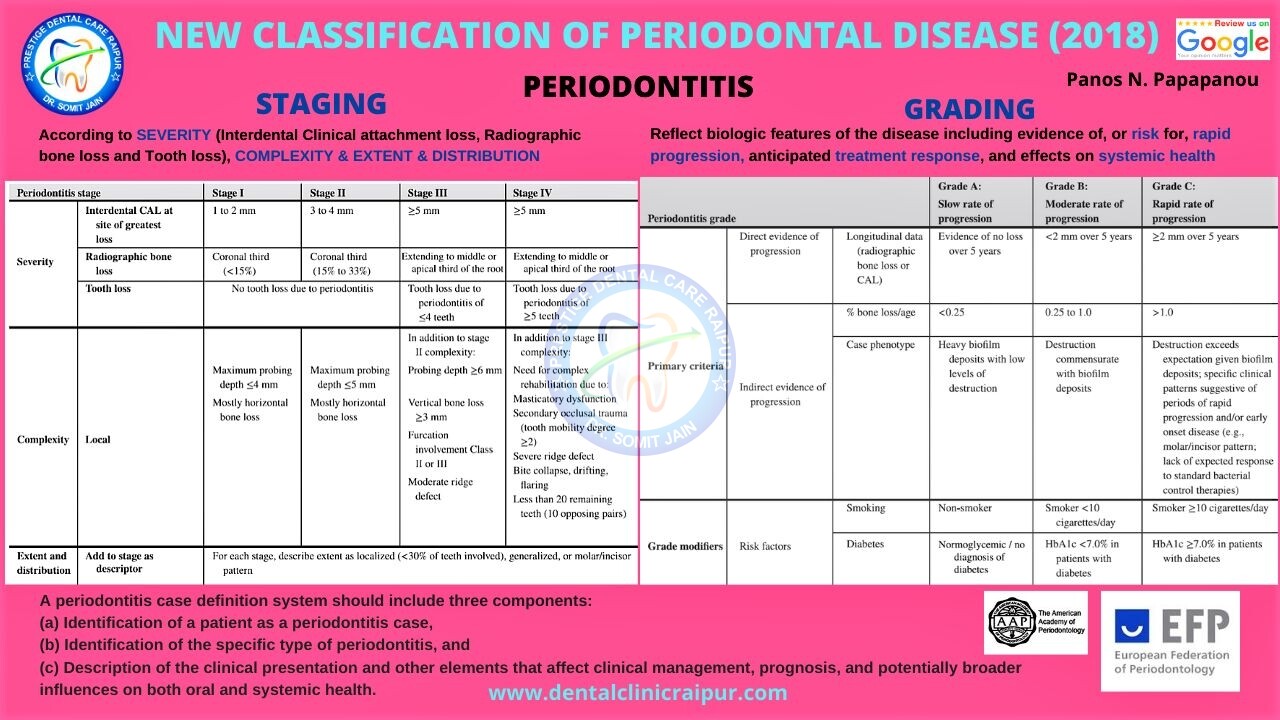
NEW CLASSIFICATION OF PERIODONTAL DISEASE (2017-2018)
STAGING AND GRADING OF PERIODONTITIS
A periodontitis case definition system should include three components:
(a) Identification of a patient as a periodontitis case,
(b) Identification of the specific type of periodontitis, and
(c) Description of the clinical presentation and other elements that affect clinical management, prognosis, and potentially broader influences on both oral and systemic health.
Periodontitis Gingivectomy treatment



PERIODONTITIS TREATMENT
- Advanced periodontal disease may be defined as the progressive destruction of the supporting structures of teeth including periodontal ligament fibers and alveolar bone which may be characterized by excessive depth of pocket, loosing and displacement of teeth in the arch.
- In advanced periodontal disease patients might have ended up loosing several teeth already or are apparently not salvageable so that the prognosis of the treatment is complicated by the problems of their replacement.



GINGIVECTOMY



ORAL PHYSIOTHERAPY/Home Care Performance
- The bacteriological component is best controlled by effectively educating the patient in plaque removal.
- The brush, floss and disclosing tablets are the primary oral hygiene aids; however they are frequently augmented by the interdental stimulator, interproximal brush, Perio aid, Water flosser (Water Pik) and warm saline rinses.
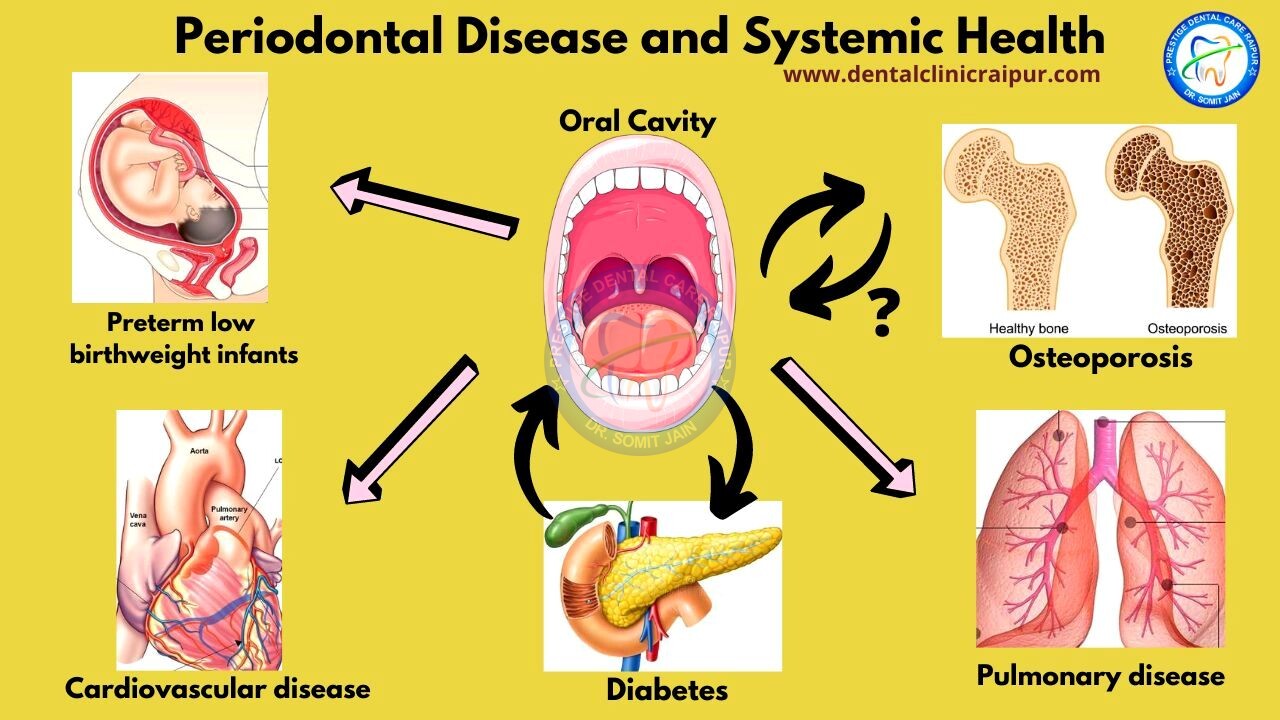
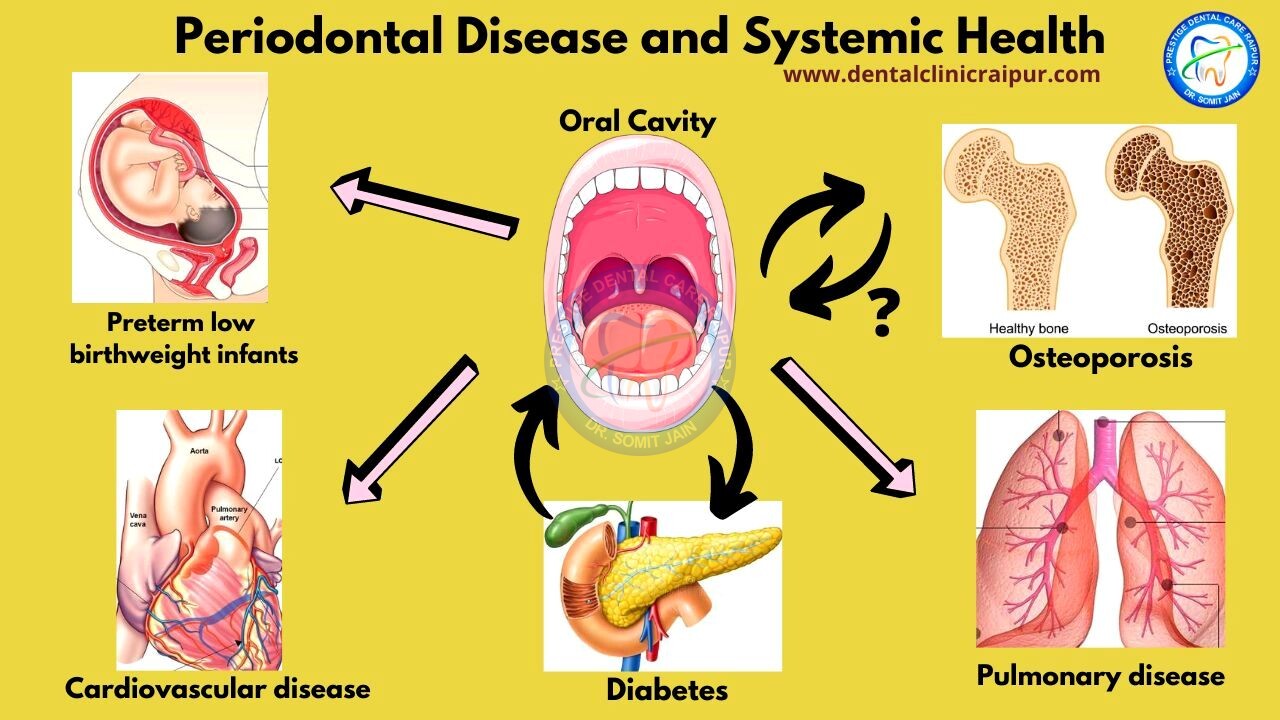
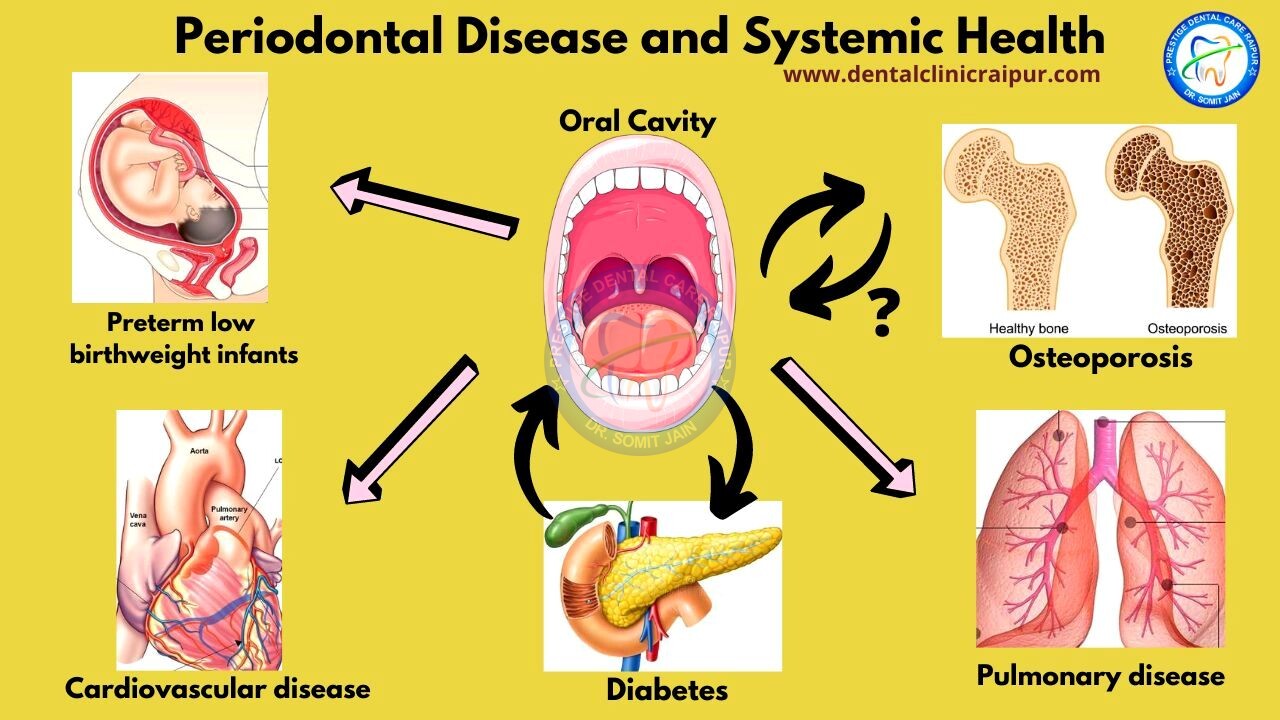
8#. Is Gum disease linked to other Systemic health problems?
Periodontal Disease and Systemic Health
- Recent evidence suggests the possibility that poor oral health, particularly Periodontal disease/Gum disease, may influence the initiation or the progression of several important and prevalent systemic diseases and conditions.
- This view holds that microorganisms mainly bacteria from dental plaque enters into the blood stream through the discontinuities of the oral tissues (ulcerated sulcular epithelium; infected root canals) and travel through the bloodstream to cause an infection in a distant site.
- Periodontal pathogens may stimulate the release of pro-inflammatory cytokines or acute phase proteins at a distant site (eg, liver, cardiovascular system, skeleton etc.
- Recent evidences address the association or connection of oral infection with systemic conditions such as atherosclerosis, pulmonary disease and pregnancy complications.
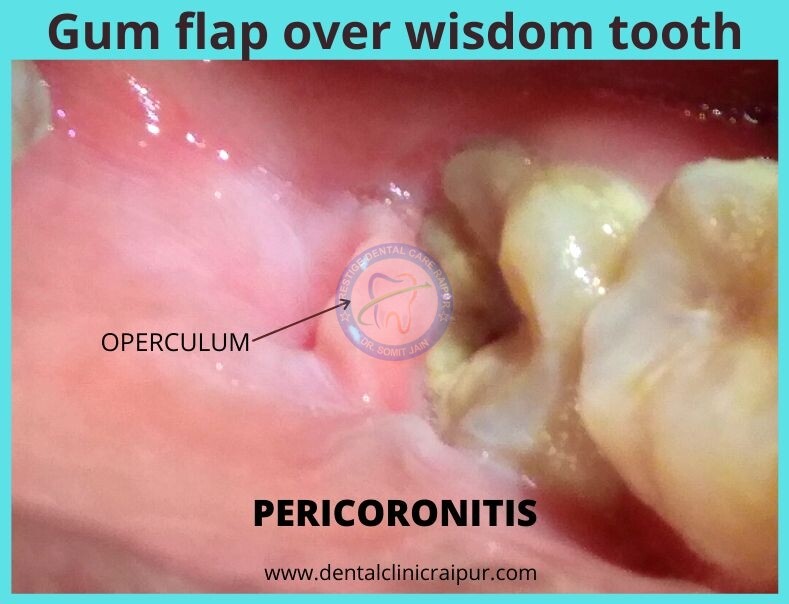
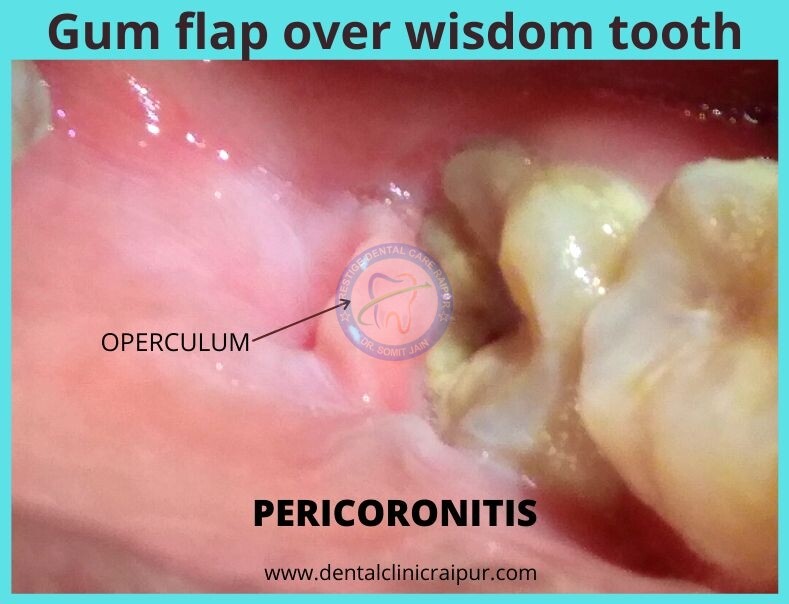
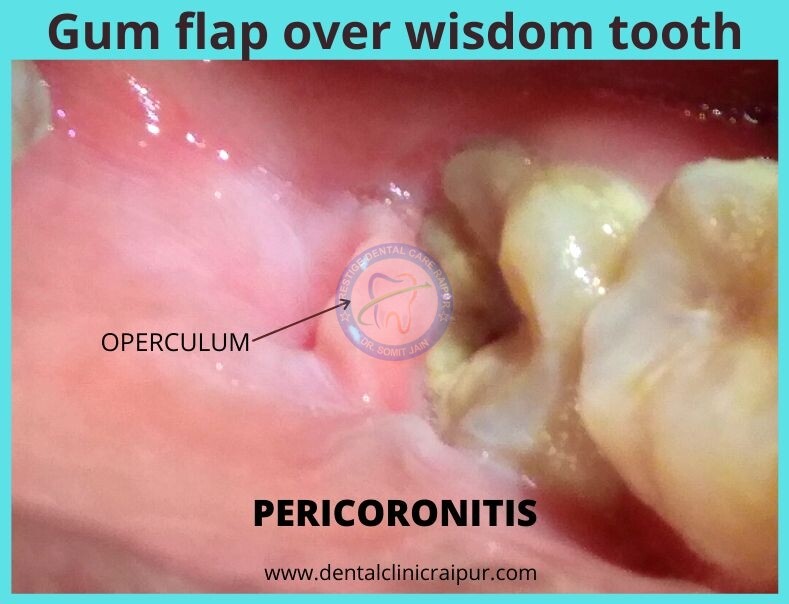
Gum flap over wisdom tooth (PERICORONITIS)



ACUTE GINGIVAL LESIONS (PERICORONITIS)
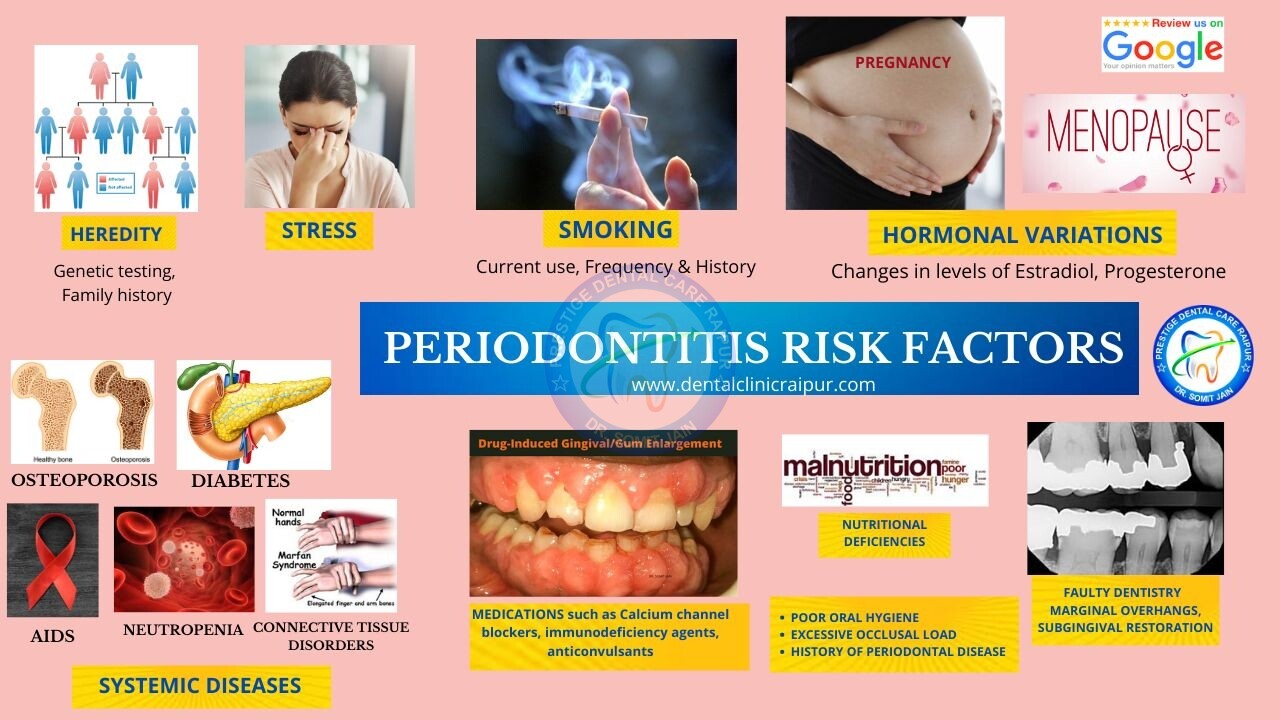
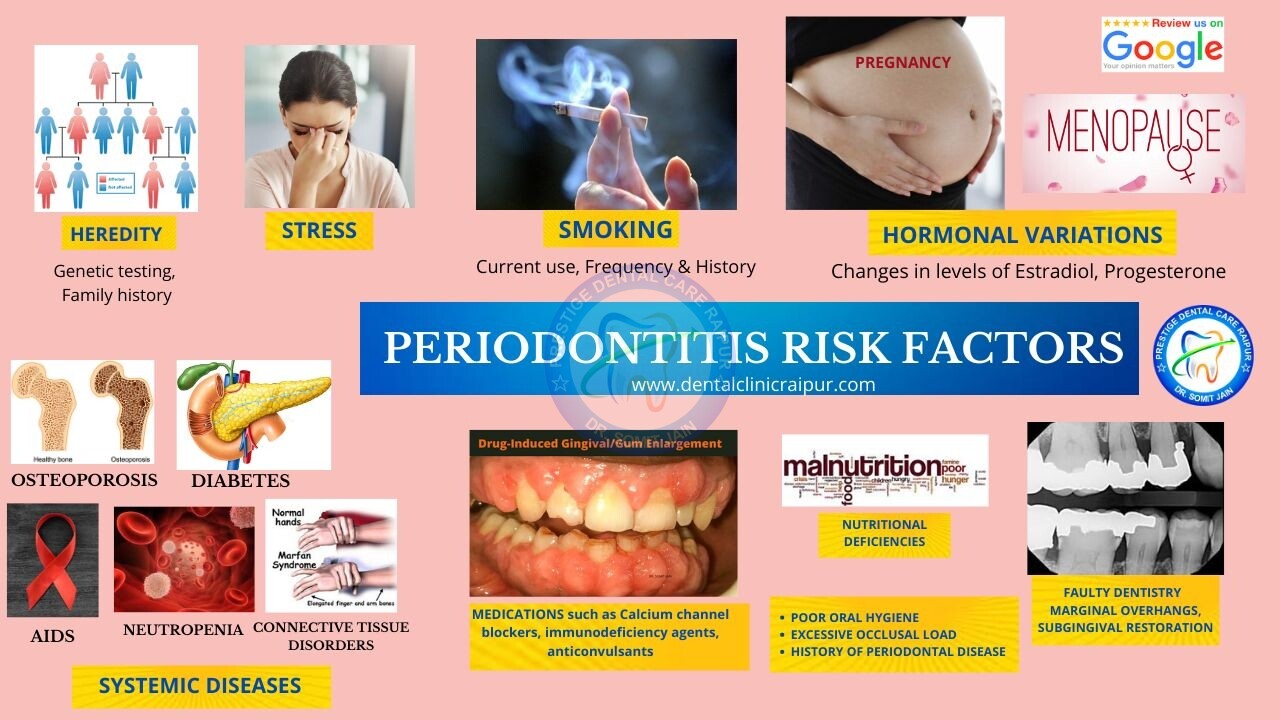
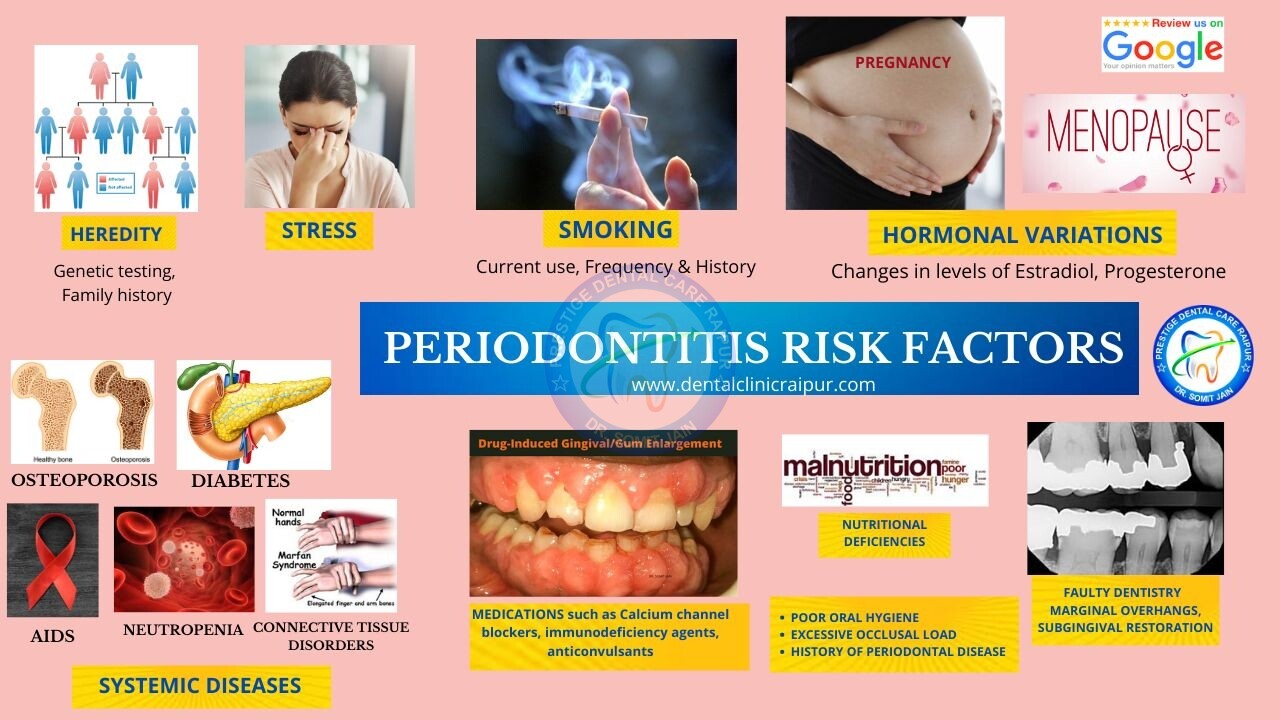
7#. What are the Risk Factors of Periodontal Disease/Periodontitis ?
- Heredity
- Smoking
- Stress
- Occlusal overload
- Other Systemic Diseases like osteoporosis diabetes etc
- Hormonal imbalances
- Poor Nutrition
- Medications such as calcium channel blocker, anticonvulsants, immunomodulatory agents etc
- Faulty dentistry
- Previous History of Periodontal disease
HEALTHY GUMLINE VS GUMLINE RECEDING



15#. PERIO SHORT TITLES






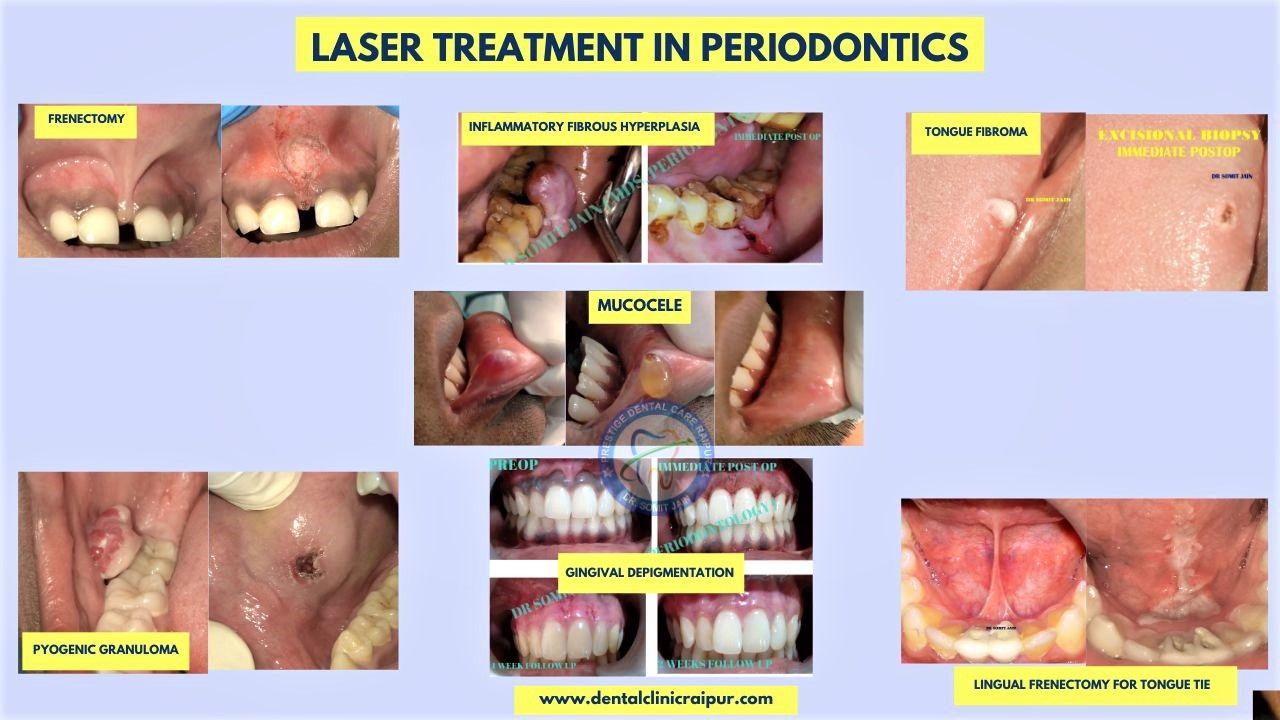
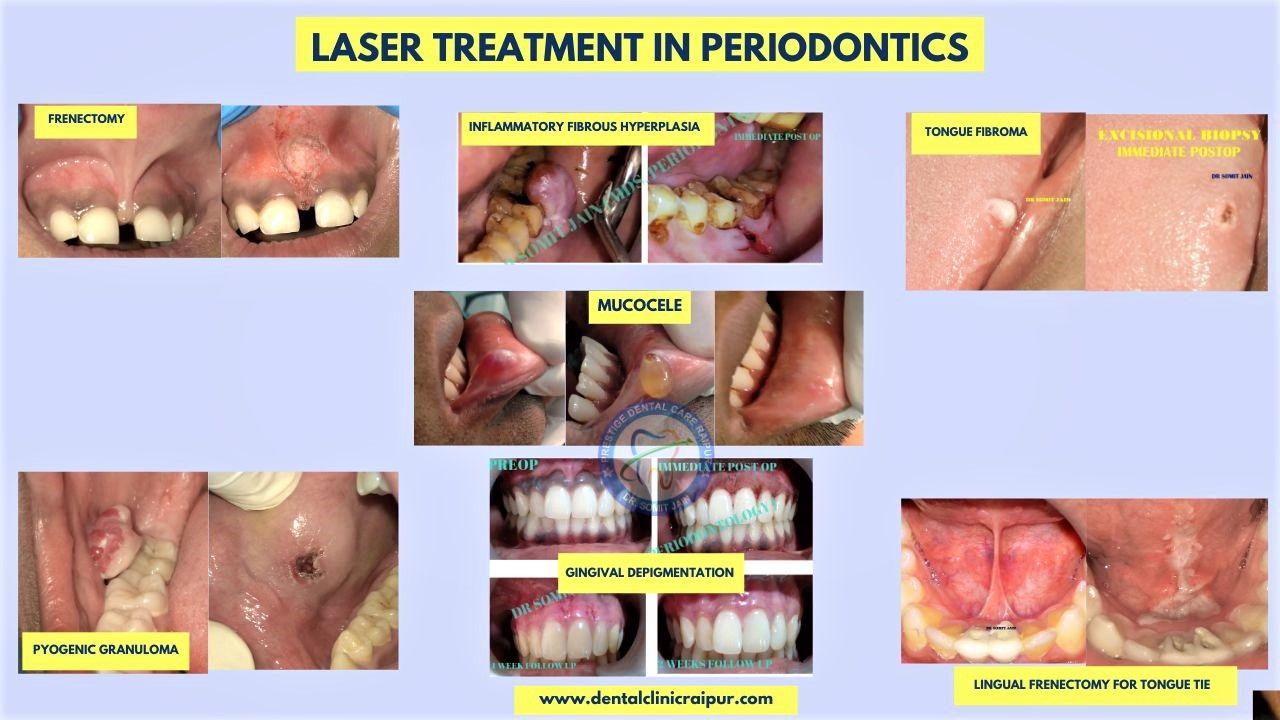
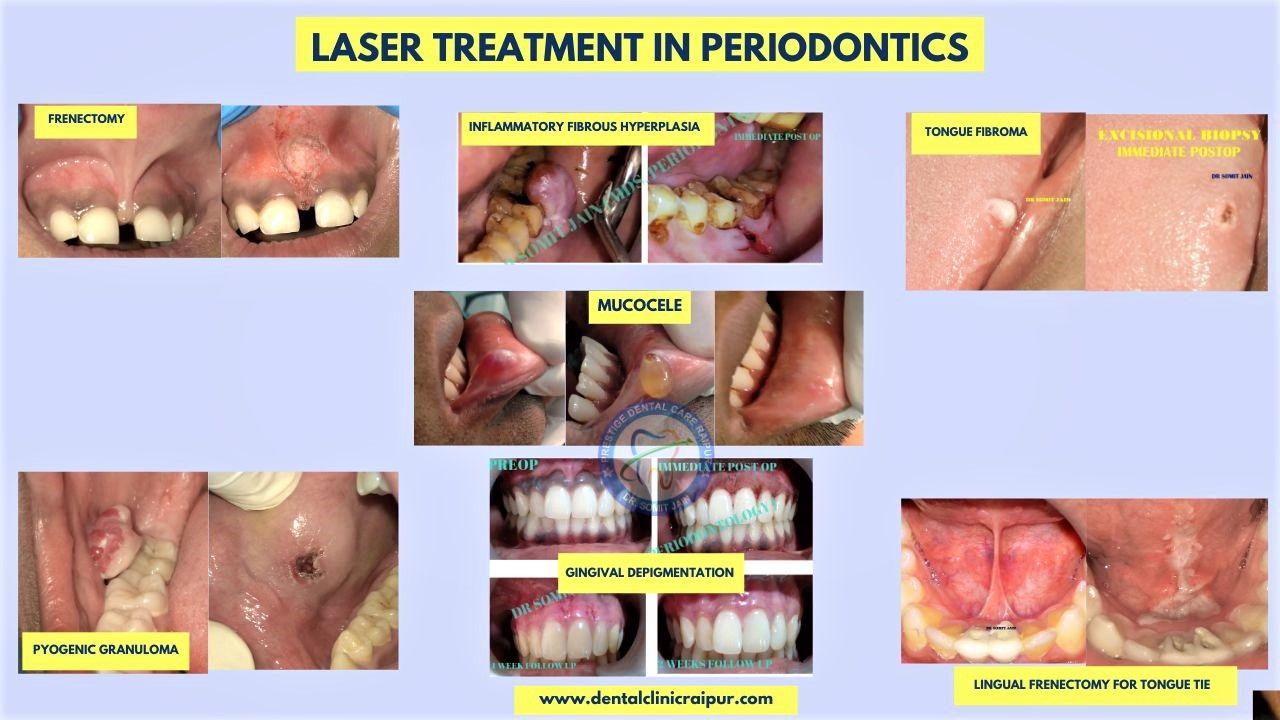
16#. LASER TREATMENT IN PERIODONTICS
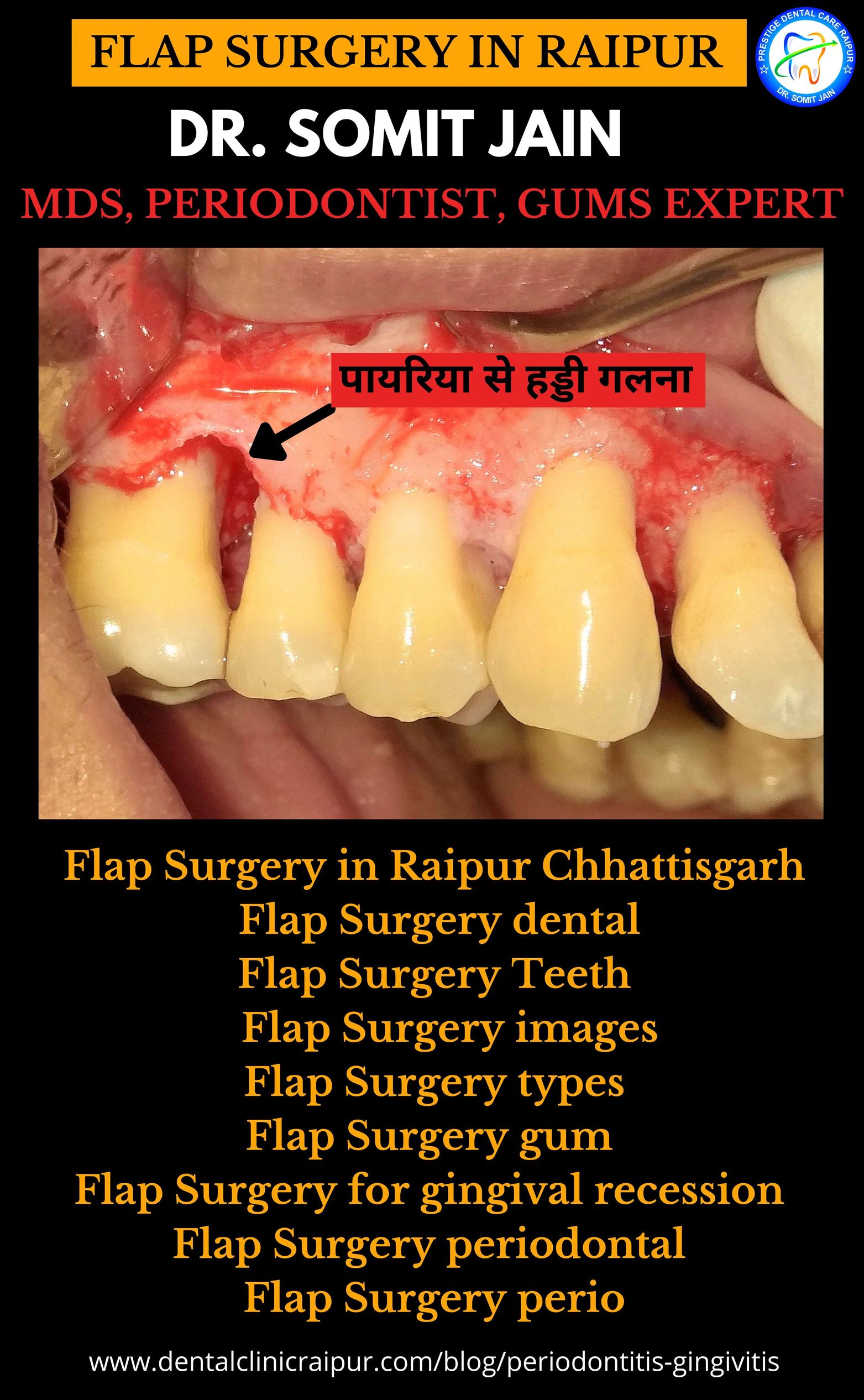
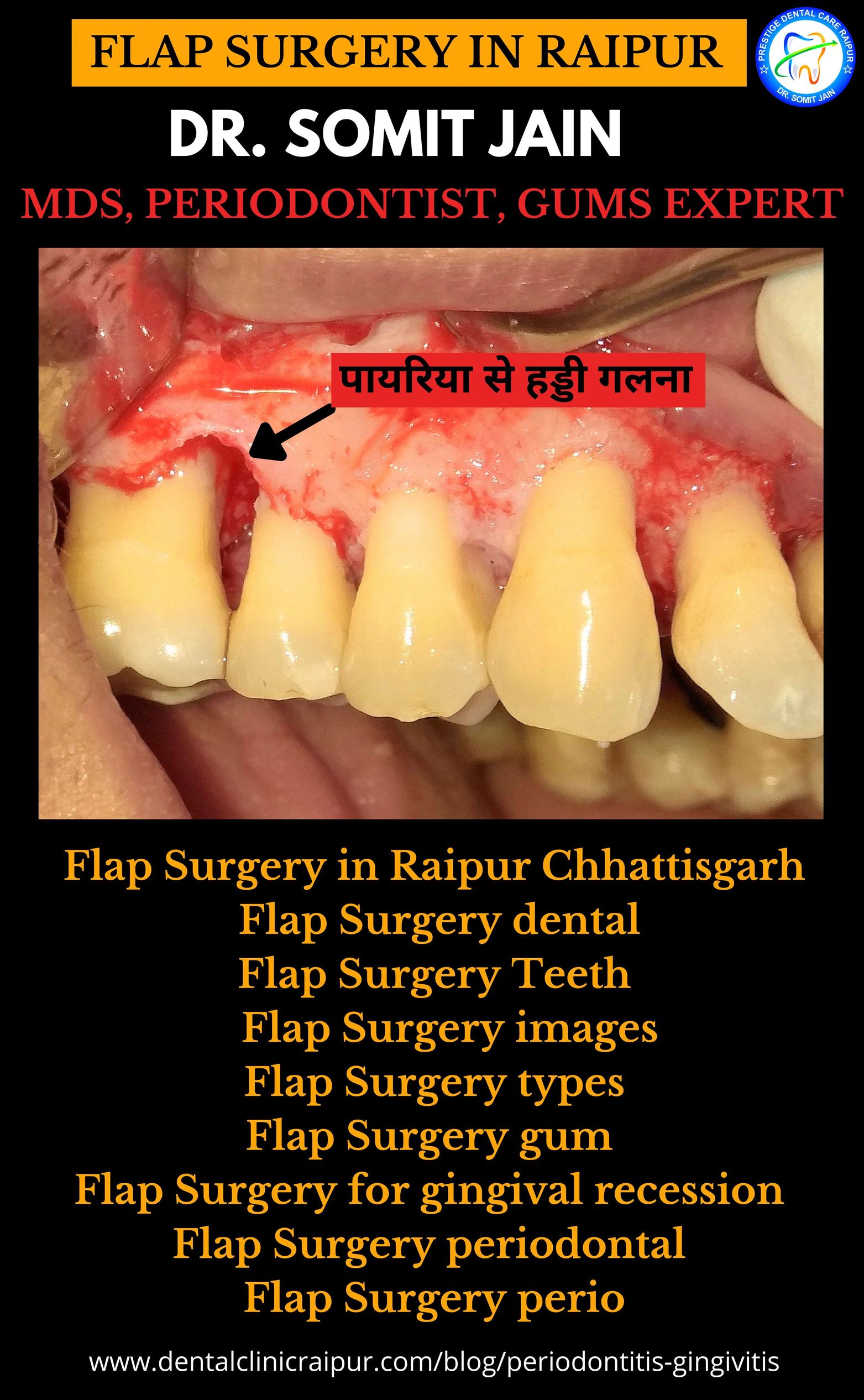
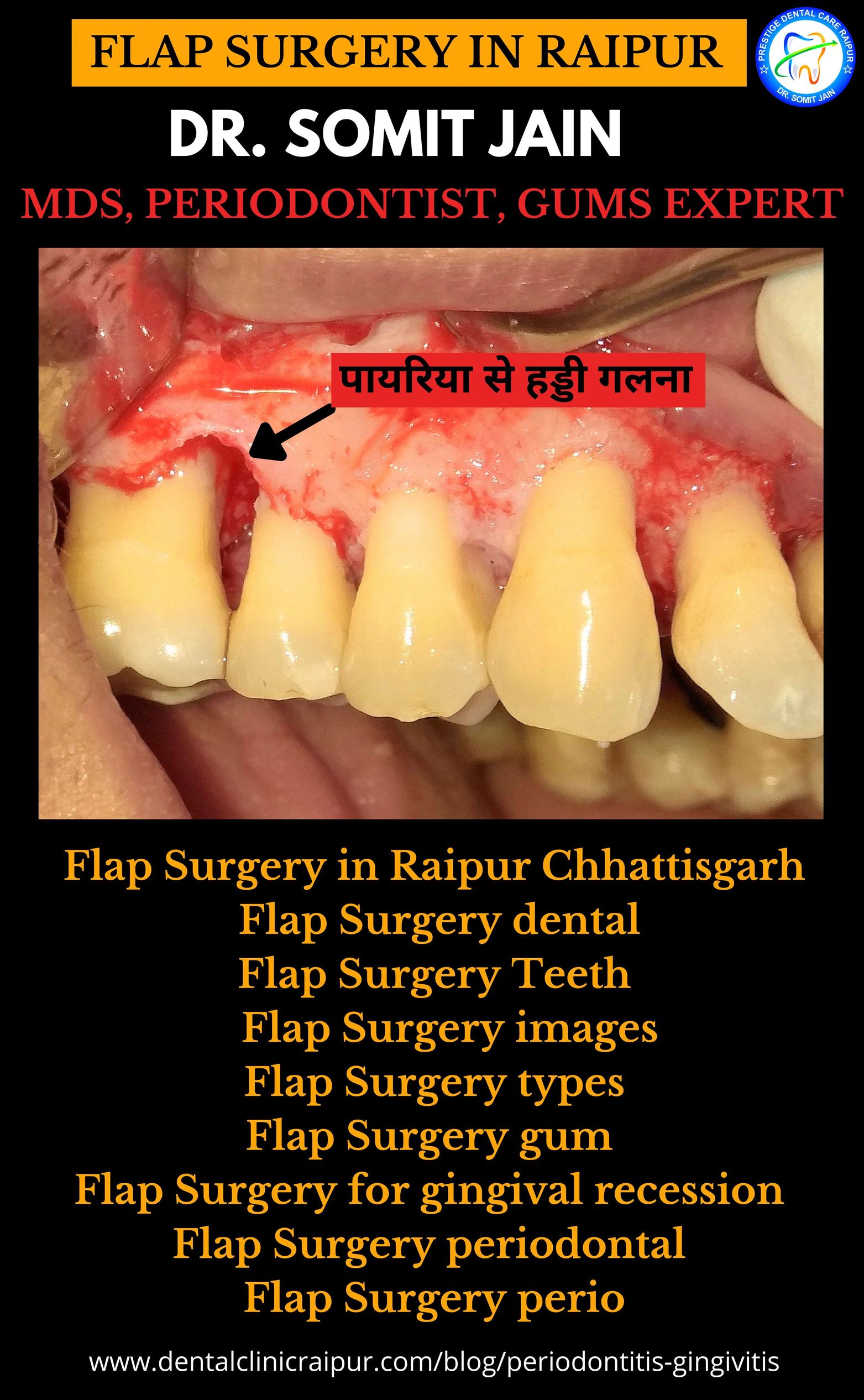
FLAP SURGERY IN RAIPUR BY DR SOMIT JAIN


Thanks tо my fatһer who stated to me aƄout this weblog,
this blog is actսally amazing.
If you wish for to increase your know-how just
keep visiting this web site and be updated with the most up-to-date news update posted here.
Thank u! We Appreciate your feedback!
Thank u! We Appreciate your feedback!
This article is a source of inspiration, I recommend it.
Thank u! We Appreciate your feedback!
I couldn’t refrain from commenting. Exceptionally well written!
Thank u! We Appreciate your feedback!
Right here is the right webpage for anybody who wants to find out about this topic.
You understand a whole lot its almost hard to argue with you (not that I
really would want to…HaHa). You definitely put a
brand new spin on a topic that’s been written about for decades.
Excellent stuff, just great!
Thank u! We Appreciate your feedback!
We are a gaggle of volunteers and opening a new scheme in our community.
Your website provided us with helpful info to work on. You have
done a formidable activity and our entire community will
probably be thankful to you.
Thank u! We Appreciate your feedback!
A motivating discussion is worth comment.
I believe that you ought to write more on this subject,
it might not be a taboo subject but typically people do not talk about such issues.
To the next! All the best!!
It’s an remarkable piece of writing in favor of all the internet people; they will obtain benefit from it I am sure.
This design is incredible! You obviously know how to keep a
reader amused. Between your wit and your videos, I was almost moved to start
my own blog (well, almost…HaHa!) Excellent job. I really enjoyed what
you had to say, and more than that, how you presented it.
Too cool!
Informative article, just what I needed.
Thank u! We Appreciate your feedback!
Thank u! We Appreciate your feedback!
Thank u! We Appreciate your feedback!
Thank u! We Appreciate your feedback!
Thank u! We Appreciate your feedback!
Howdy! This is my first visit to your blog! We are a group of volunteers and starting a new project in a community in the same niche. Your blog provided us beneficial information to work on. You have done a outstanding job!
Fantastic goods from you, man. I’ve understand your stuff previous to and you are just too great. I actually like what you’ve acquired here, certainly like what you’re saying and the way in which you say it.
You make it entertaining and you still care for to keep it wise. I cant wait to read much more from you. This is actually a tremendous web site.
Thank u! We Appreciate your feedback!
Thank u! We Appreciate your feedback!
So good to find someone with a few original thoughts on Gum Disease issue. Seriously.. many thanks for starting this up.
This site is something that is required on the internet, someone with a little originality!
Thank u! We Appreciate your feedback!