THE PERIODONTAL POCKET/DENTAL POCKET/GUM POCKETS/TEETH POCKET/POCKET FORMATION/TEETH GUM POCKETS/ PSUDOPOCKETS
WHAT DO PERIODONTAL POCKET LOOK LIKE..??
DEFINITION:
- The Periodontal pocket is defined as a pathologically deepened gingiva sulcus.
- A Periodontal Pocket is a fissure between the cementum and the epithelium and is created by the destruction of periodontal attachment apparatus.
- Periodontal Pocket is roentgenolucent and not recorded on x-ray.
How to probe the periodontal pocket.??
Pockets are found by probing the gingival crevice around the entire circumference of the tooth.
Pocket depth can be recorded on the x-ray by inserting roentgenopaque material such as Gutta-Percha points into the pocket.
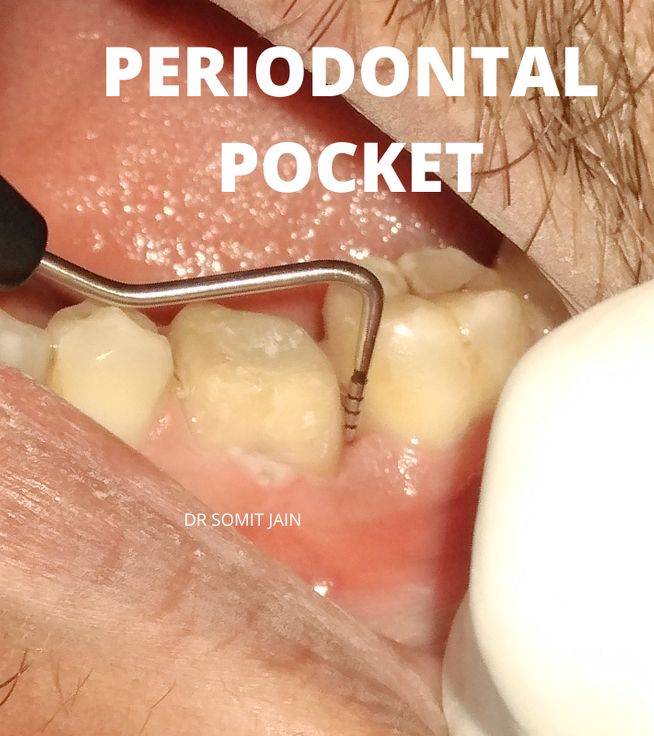
Illustration of Periodontal probing of a molar (Infrabony Pocket depth here recorded was 11 mm)